Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
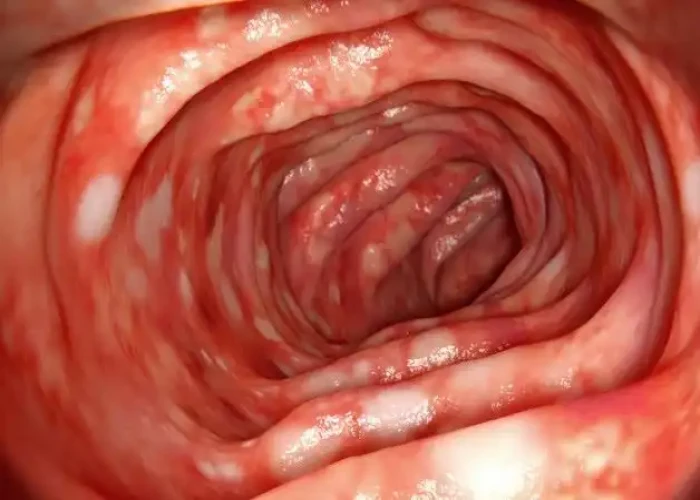
Ulcerative colitis
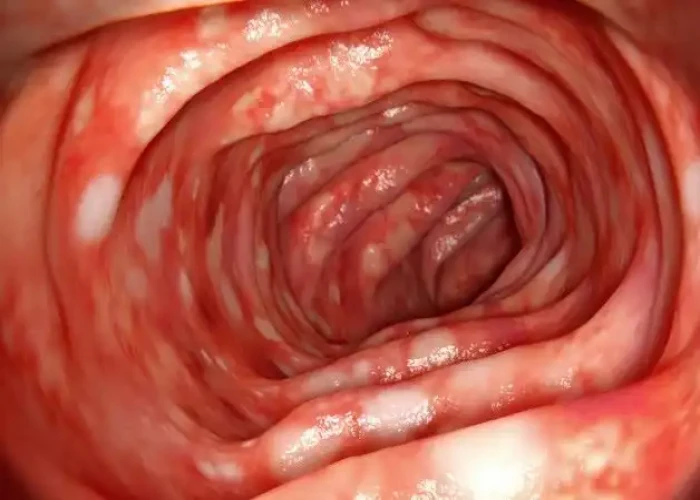
Ulcerative colitis is a chronic inflammatory bowel disease that affects the large intestine (colon) and rectum. The exact cause of ulcerative colitis is not known, but it is believed to be an autoimmune condition, in which the body's immune system attacks the lining of the colon, causing inflammation and ulcers.
The symptoms of ulcerative colitis can vary in severity and may include abdominal pain, diarrhea, rectal bleeding, weight loss, and fatigue. Some people may also experience complications such as anemia, dehydration, and inflammation of other parts of the body such as the joints, eyes, and skin.
Treatment for ulcerative colitis aims to reduce inflammation and manage symptoms. This may include medication such as anti-inflammatory drugs, immunosuppressants, and biologics, as well as dietary changes, stress management, and surgery in severe cases. It is important to work closely with a healthcare provider to develop an individualized treatment plan based on the severity and location of the inflammation.
Living with ulcerative colitis can be challenging, and it is important to manage the condition to prevent complications and improve quality of life. This may include making lifestyle changes such as reducing stress, getting regular exercise, and avoiding foods that trigger symptoms. Support groups and counseling can also be helpful for managing the emotional impact of the condition. Regular check-ups with a healthcare provider are important to monitor the condition and adjust the treatment plan as needed.
Research Papers
Disease Signs and Symptoms
- Diarrhea
- Abdomen pain
- Abdomen cramps
- Anus pain
- Anus bleeding
- Weight loss
- Fatigue (Tiredness)
- Fever
- Rectal bleeding — passing small amount of blood with stool
Disease Causes
Ulcerative colitis
The exact cause of ulcerative colitis remains unknown. Previously, diet and stress were suspected, but now doctors know that these factors may aggravate but don't cause ulcerative colitis.
One possible cause is an immune system malfunction. When your immune system tries to fight off an invading virus or bacterium, an abnormal immune response causes the immune system to attack the cells in the digestive tract, too.
Heredity also seems to play a role in that ulcerative colitis is more common in people who have family members with the disease. However, most people with ulcerative colitis don't have this family history.
Disease Prevents
Disease Treatments
Ulcerative colitis treatment usually involves either drug therapy or surgery.
Several categories of drugs may be effective in treating ulcerative colitis. The type you take will depend on the severity of your condition. The drugs that work well for some people may not work for others, so it may take time to find a medication that helps you.
In addition, because some drugs have serious side effects, you'll need to weigh the benefits and risks of any treatment.
Anti-inflammatory drugs
Anti-inflammatory drugs are often the first step in the treatment of ulcerative colitis and are appropriate for the majority of people with this condition. These drugs include:
- 5-aminosalicylates. Examples of this type of medication include sulfasalazine (Azulfidine), mesalamine (Asacol HD, Delzicol, others), balsalazide (Colazal) and olsalazine (Dipentum). Which one you take, and whether it is taken by mouth or as an enema or suppository, depends on the area of your colon that's affected.
- Corticosteroids. These drugs, which include prednisone and budesonide, are generally reserved for moderate to severe ulcerative colitis that doesn't respond to other treatments. Due to the side effects, they are not usually given long term.
Immune system suppressors
These drugs also reduce inflammation, but they do so by suppressing the immune system response that starts the process of inflammation. For some people, a combination of these drugs works better than one drug alone.
Immunosuppressant drugs include:
- Azathioprine (Azasan, Imuran) and mercaptopurine (Purinethol, Purixan). These are the most widely used immunosuppressants for the treatment of inflammatory bowel disease. Taking them requires that you follow up closely with your doctor and have your blood checked regularly to look for side effects, including effects on the liver and pancreas.
- Cyclosporine (Gengraf, Neoral, Sandimmune). This drug is normally reserved for people who haven't responded well to other medications. Cyclosporine has the potential for serious side effects and is not for long-term use.
- Tofacitinib (Xeljanz). This is called a "small molecule" and works by stopping the process of inflammation. Tofacitinib is effective when other therapies don't work. Main side effects include the increased risk of shingles infection and blood clots.
- The U.S. Food and Drug Administration (FDA) recently issued a warning about tofacitinib, stating that preliminary studies show an increased risk of serious heart-related problems and cancer from taking this drug. If you're taking tofacitinib for ulcerative colitis, don't stop taking the medication without first talking with your doctor.
Biologics
This class of therapies targets proteins made by the immune system. Types of biologics used to treat ulcerative colitis include:
- Infliximab (Remicade), adalimumab (Humira) and golimumab (Simponi). These drugs, called tumor necrosis factor (TNF) inhibitors, or biologics, work by neutralizing a protein produced by your immune system. They are for people with severe ulcerative colitis who don't respond to or can't tolerate other treatments.
- Vedolizumab (Entyvio). This medication is approved for treatment of ulcerative colitis for people who don't respond to or can't tolerate other treatments. It works by blocking inflammatory cells from getting to the site of inflammation.
- Ustekinumab (Stelara). This medication is approved for treatment of ulcerative colitis for people who don't respond to or can't tolerate other treatments. It works by blocking a different protein that causes inflammation.
Other medications
You may need additional medications to manage specific symptoms of ulcerative colitis. Always talk with your doctor before using over-the-counter medications. He or she may recommend one or more of the following.
- Anti-diarrheal medications. For severe diarrhea, loperamide (Imodium A-D) may be effective. Use anti-diarrheal medications with great caution and after talking with your doctor, because they may increase the risk of an enlarged colon (toxic megacolon).
- Pain relievers. For mild pain, your doctor may recommend acetaminophen (Tylenol, others) — but not ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve) and diclofenac sodium, which can worsen symptoms and increase the severity of disease.
- Antispasmodics. Sometimes doctors will prescribe antispasmodic therapies to help with cramps.
- Iron supplements. If you have chronic intestinal bleeding, you may develop iron deficiency anemia and be given iron supplements.
Surgery
Surgery can eliminate ulcerative colitis and involves removing your entire colon and rectum (proctocolectomy).
In most cases, this involves a procedure called ileoanal anastomosis (J-pouch) surgery. This procedure eliminates the need to wear a bag to collect stool. Your surgeon constructs a pouch from the end of your small intestine. The pouch is then attached directly to your anus, allowing you to expel waste relatively normally.
In some cases a pouch is not possible. Instead, surgeons create a permanent opening in your abdomen (ileal stoma) through which stool is passed for collection in an attached bag.
Cancer surveillance
You will need more-frequent screening for colon cancer because of your increased risk. The recommended schedule will depend on the location of your disease and how long you have had it. People with proctitis are not at increased risk of colon cancer.
If your disease involves more than your rectum, you will require a surveillance colonoscopy every one to two years, beginning as soon as eight years after diagnosis if the majority of your colon is involved, or 15 years if only the left side of your colon is involved.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Ulcerative colitis and Learn More about Diseases

Nightmare disorder

Pectus carinatum

Rett syndrome

Hemophilia

Chronic daily headaches

Oral thrush

Dust mite allergy

Sciatica
ulcerative colitis, আলসারেটিভ কোলাইটিস
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.