Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
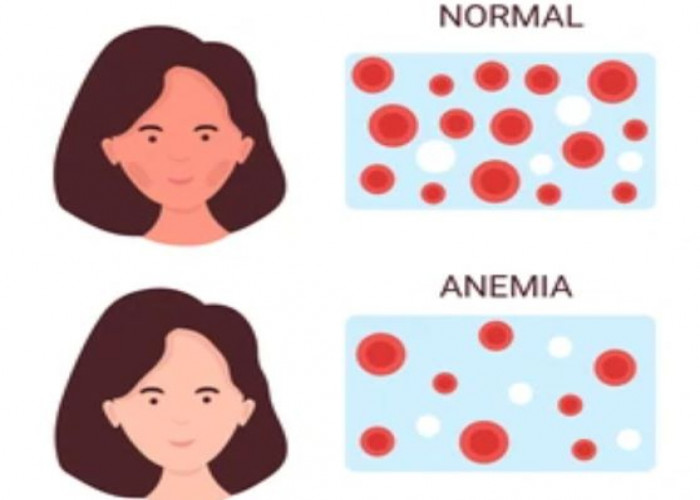
Aplastic anemia
Aplastic anemia is a rare and serious condition in which the body stops producing enough new blood cells. This leads to a shortage of red blood cells, which carry oxygen to the body's tissues, white blood cells, which help fight infections, and platelets, which are important for blood clotting.
Aplastic anemia can be caused by a variety of factors, including exposure to toxic chemicals, certain medications, radiation therapy, and viral infections. In some cases, the cause of aplastic anemia is unknown.
Symptoms of aplastic anemia can include fatigue, weakness, shortness of breath, pale skin, easy bruising or bleeding, and frequent infections. The condition can also cause complications such as anemia, increased risk of bleeding, and a decreased ability to fight infections.
Treatment for aplastic anemia depends on the severity of the condition and the presence of any underlying cause. In mild cases, medication to stimulate blood cell production may be sufficient to manage symptoms. In more severe cases, treatment may include a bone marrow transplant, which replaces the damaged bone marrow with healthy bone marrow from a donor.
It is important to seek medical attention if you experience symptoms of aplastic anemia, as prompt treatment can help prevent serious complications and improve outcomes. Your doctor can perform tests to determine the cause and severity of your condition and recommend the best course of treatment for you.
Research Papers
Disease Signs and Symptoms
- Fatigue (Tiredness)
- Headaches
- Dizziness (vertigo)
- Skin rash
- Prolonged bleeding from minor cuts
- Unusual bleeding, such as a nosebleed or bleeding gums
- Easy bruising or unexplained bruises
- Frequent and prolonged infections
- Pale skin color (pallor)
- Irregular heartbeats (arrhythmia)
- Shortness of breath (dyspnea)
- Fever
Disease Causes
Aplastic anemia
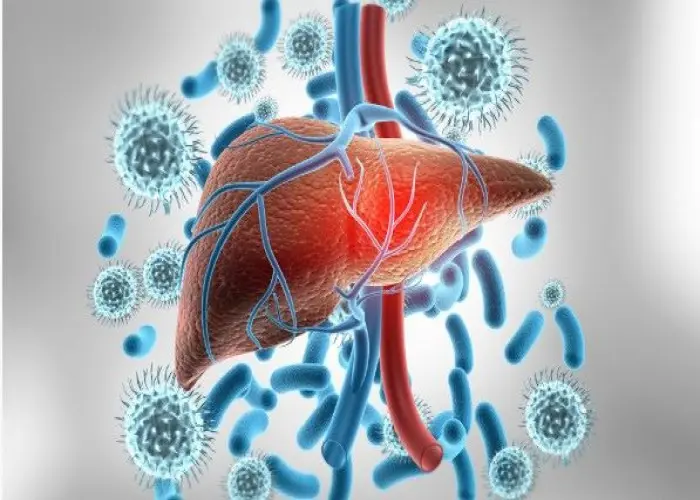
Stem cells in the bone marrow produce blood cells — red cells, white cells and platelets. In aplastic anemia, stem cells are damaged. As a result, the bone marrow is either empty (aplastic) or contains few blood cells (hypoplastic).
The most common cause of aplastic anemia is from your immune system attacking the stem cells in your bone marrow. Other factors that can injure bone marrow and affect blood cell production include:
- Radiation and chemotherapy treatments. While these cancer-fighting therapies kill cancer cells, they can also damage healthy cells, including stem cells in bone marrow. Aplastic anemia can be a temporary side effect of these treatments.
- Exposure to toxic chemicals. Toxic chemicals, such as some used in pesticides and insecticides, and benzene, an ingredient in gasoline, have been linked to aplastic anemia. This type of anemia might improve if you avoid repeated exposure to the chemicals that caused your illness.
- Use of certain drugs. Some medications, such as those used to treat rheumatoid arthritis and some antibiotics, can cause aplastic anemia.
- Autoimmune disorders. An autoimmune disorder, in which your immune system attacks healthy cells, might involve stem cells in your bone marrow.
- A viral infection. Viral infections that affect bone marrow can play a role in the development of aplastic anemia. Viruses that have been linked to aplastic anemia include hepatitis, Epstein-Barr, cytomegalovirus, parvovirus B19 and HIV.
- Pregnancy. Your immune system might attack your bone marrow during pregnancy.
- Unknown factors. In many cases, doctors aren't able to identify the cause of aplastic anemia (idiopathic aplastic anemia).
Connections with other rare disorders
Some people with aplastic anemia also have a rare disorder known as paroxysmal nocturnal hemoglobinuria, which causes red blood cells to break down too soon. This condition can lead to aplastic anemia, or aplastic anemia can evolve into paroxysmal nocturnal hemoglobinuria.
Fanconi's anemia is a rare, inherited disease that leads to aplastic anemia. Children born with it tend to be smaller than average and have birth defects, such as underdeveloped limbs. The disease is diagnosed with the help of blood tests.
Disease Prevents
Disease Treatments
Treatments for aplastic anemia, which will depend on the severity of your condition and your age, might include observation, blood transfusions, medications, or bone marrow transplantation. Severe aplastic anemia, in which your blood cell counts are extremely low, is life-threatening and requires immediate hospitalization.
Blood transfusions
Although not a cure for aplastic anemia, blood transfusions can control bleeding and relieve symptoms by providing blood cells your bone marrow isn't producing. You might receive:
- Red blood cells. These raise red blood cell counts and help relieve anemia and fatigue.
- Platelets. These help prevent excessive bleeding.
While there's generally no limit to the number of blood transfusions you can have, complications can sometimes arise with multiple transfusions. Transfused red blood cells contain iron that can accumulate in your body and can damage vital organs if an iron overload isn't treated. Medications can help rid your body of excess iron.
Over time your body can develop antibodies to transfused blood cells, making them less effective at relieving symptoms. The use of immunosuppressant medication makes this complication less likely.
Stem cell transplant
A stem cell transplant to rebuild the bone marrow with stem cells from a donor might be the only successful treatment option for people with severe aplastic anemia. A stem cell transplant, also called a bone marrow transplant, is generally the treatment of choice for people who are younger and have a matching donor — most often a sibling.
If a donor is found, your diseased bone marrow is first depleted with radiation or chemotherapy. Healthy stem cells from the donor are filtered from the blood. The healthy stem cells are injected intravenously into your bloodstream, where they migrate to the bone marrow cavities and begin creating new blood cells.
The procedure requires a lengthy hospital stay. After the transplant, you'll receive drugs to help prevent rejection of the donated stem cells.
A stem cell transplant carries risks. Your body may reject the transplant, leading to life-threatening complications. In addition, not everyone is a candidate for transplantation or can find a suitable donor.
Immunosuppressants
For people who can't undergo a bone marrow transplant or for those whose aplastic anemia is due to an autoimmune disorder, treatment can involve drugs that alter or suppress the immune system (immunosuppressants).
Drugs such as cyclosporine (Gengraf, Neoral, Sandimmune) and anti-thymocyte globulin suppress the activity of immune cells that are damaging your bone marrow. This helps your bone marrow recover and generate new blood cells. Cyclosporine and anti-thymocyte globulin are often used together.
Corticosteroids, such as methylprednisolone (Medrol, Solu-Medrol), are often used with these drugs.
Although effective, these drugs further weaken your immune system. It's also possible for anemia to return after you stop these drugs.
Bone marrow stimulants
Certain drugs — including colony-stimulating factors, such as sargramostim (Leukine), filgrastim (Neupogen) and pegfilgrastim (Neulasta), epoetin alfa (Epogen/Procrit), and eltrombopag (Promacta) — help stimulate the bone marrow to produce new blood cells. Growth factors are often used with immune-suppressing drugs.
Antibiotics, antivirals
Having aplastic anemia weakens your immune system, which leaves you more prone to infections.
If you have aplastic anemia, see your doctor at the first sign of infection, such as a fever. You don't want the infection to get worse, because it could prove life-threatening. If you have severe aplastic anemia, your doctor might prescribe antibiotics or antiviral medications to help prevent infections.
Other treatments
Aplastic anemia caused by radiation and chemotherapy treatments for cancer usually improves after those treatments stop. The same is true for most other drugs that induce aplastic anemia.
Pregnant women with aplastic anemia are treated with blood transfusions. For many women, pregnancy-related aplastic anemia improves once the pregnancy ends. If that doesn't happen, treatment is still necessary.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Aplastic anemia and Learn More about Diseases
Hepatitis C
Pancreatic cysts
Absence seizure

Lung Abesess
Thunderclap headaches
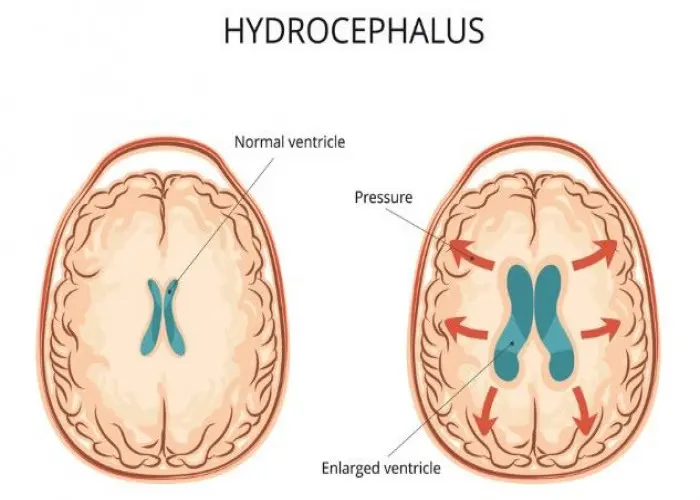
Hydrocephalus

Staph infections

Pediatric white blood cell disorders
Aplastic anemia, Aplastic, Aplastic anemia symptoms, Aplastic crisis, অ্যাপ্লাস্টিক অ্যানেমিয়া
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.