Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
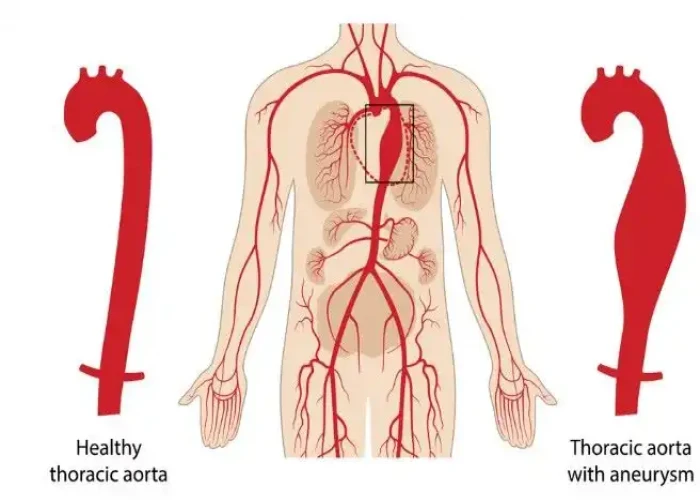
Thoracic aortic aneurysm
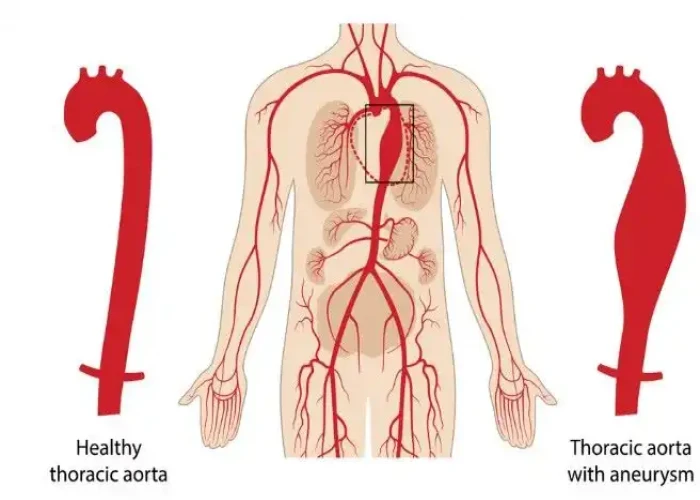
A thoracic aortic aneurysm (TAA) is a weakened and bulging area in the wall of the aorta, the main blood vessel that carries oxygen-rich blood from the heart to the rest of the body. TAAs are located in the section of the aorta that runs through the chest, called the thoracic aorta.
TAAs can be caused by a variety of factors, including genetics, high blood pressure, and connective tissue disorders. They often have no symptoms and are usually discovered incidentally when a medical imaging test is done for another reason.
However, as the aneurysm grows, it can put pressure on surrounding organs and tissues, leading to symptoms such as chest pain, back pain, and shortness of breath. If a TAA ruptures, it can cause life-threatening bleeding and requires immediate medical attention.
The treatment for a TAA depends on its size and location, as well as the patient's age and overall health. For smaller TAAs, the patient may be monitored regularly with imaging tests and treated with medication to control blood pressure and reduce the risk of rupture. For larger TAAs or those that are growing rapidly, surgery may be recommended to repair or replace the weakened section of the aorta.
Prevention of a TAA involves managing risk factors such as high blood pressure, smoking, and connective tissue disorders, as well as seeking medical attention if there is a family history of aortic aneurysms or if there are any concerning symptoms.
Research Papers
Disease Signs and Symptoms
- Chest pain
- Back pain
- Hoarseness
- Cough
- Shortness of breath (dyspnea)
- Jaw pain
- Neck pain
- Arm or Hand pain
- Difficulty breathing (dyspnea)
Disease Causes
Thoracic aortic aneurysm
Factors that can contribute to an aneurysm's development include:
- Hardening of the arteries (atherosclerosis). As plaque builds up on your artery walls, they become less flexible, and the additional pressure can cause them to weaken and bulge. High blood pressure and high cholesterol are risk factors for hardening of the arteries. This is more common in older people.
- Genetic conditions. Aortic aneurysms in younger people often have a genetic cause. People who are born with Marfan syndrome, a genetic condition that affects the connective tissue in the body, are particularly at risk of a thoracic aortic aneurysm because they may have weakness in the aortic wall.
- Marfan syndrome generally causes distinct physical traits, including tall stature, very long arms, a deformed breastbone and eye problems.
- Other family-related disorders can cause an aortic aneurysm, including vascular Ehlers-Danlos, Loeys-Dietz and Turner syndromes. Vascular Ehlers-Danlos syndrome causes your skin, joints and connective tissue to be fragile and makes your skin stretch easily.
- Other medical conditions. Inflammatory conditions, such as giant cell arteritis and Takayasu arteritis, are associated with thoracic aortic aneurysms.
- Problems with your heart's aortic valve. Sometimes people who have problems with the valve that blood flows through as it leaves the heart (aortic valve) have an increased risk of thoracic aortic aneurysm. This is mainly true for people who were born with an aortic valve that has only two flaps instead of three (bicuspid aortic valve).
- Untreated infection. Though rare, it's possible to develop a thoracic aortic aneurysm if you've had an untreated infection, such as syphilis or salmonella.
- Traumatic injury. Rarely, some people who are injured in falls or motor vehicle crashes develop thoracic aortic aneurysms.
Aortic emergencies
In aortic dissection, a tear occurs in the wall of the aorta. This causes bleeding into and along the aortic wall and, in some cases, completely outside the aorta (rupture).
An aortic dissection is a potential life-threatening emergency, depending on where in the aorta it occurs. It's important to treat an aortic aneurysm to try to prevent dissection. If dissection occurs, people can still be treated with surgery, but they will have a higher risk of complications.
Disease Prevents
Disease Treatments
The goal of treatment is to prevent your aneurysm from growing and to treat it before it dissects or ruptures. Depending on the size and growth rate of your thoracic aortic aneurysm, treatment may vary from watchful waiting (monitoring) to surgery.
Monitoring
If your thoracic aortic aneurysm is small, your doctor may recommend imaging tests to monitor the aneurysm, along with medication and management of other medical conditions.
Usually, you'll have an echocardiogram, CT or magnetic resonance angiography (MRA) scan at least six months after your aneurysm is diagnosed, and at regular follow-up exams. How often you have these tests done depends on the cause and size of the aneurysm, and how fast it's growing.
Medications
If you have high blood pressure or blockages in your arteries, your doctor will likely prescribe medications to lower your blood pressure and cholesterol.
These medications could include:
- Beta blockers. Beta blockers lower your blood pressure by slowing your heart rate. For people with Marfan syndrome, beta blockers may reduce how fast the aorta is widening. Examples of beta blockers include metoprolol (Lopressor, Toprol-XL, Kapspargo Sprinkle), atenolol (Tenormin) and bisoprolol.
- Angiotensin II receptor blockers. Your doctor may also prescribe these medications if beta blockers aren't enough to control your blood pressure or if you can't take beta blockers. These medications are often recommended for people who have Marfan syndrome even if they don't have high blood pressure. Examples of angiotensin II receptor blockers include losartan (Cozaar), valsartan (Diovan) and olmesartan (Benicar).
- Statins. These medications can help lower your cholesterol, which can help reduce blockages in your arteries and reduce your risk of aneurysm complications. Examples of statins include atorvastatin (Lipitor), lovastatin (Altoprev), simvastatin (Zocor, FloLipid) and others.
If you smoke or chew tobacco, it's important that you quit. Using tobacco can worsen your aneurysm.
Surgery
Surgery is generally recommended for thoracic aortic aneurysms about 1.9 to 2.4 inches (about 5 to 6 centimeters) and larger. If you have Marfan syndrome, another connective tissue disease, a bicuspid aortic valve or a family history of aortic dissection, your doctor may recommend surgery for smaller aneurysms due to the higher risk of aortic dissection.
Most people with a thoracic aortic aneurysm have open-chest surgery, but in some select cases your doctor may determine you're a candidate for a less invasive repair called endovascular surgery.
The type of surgery you have depends on your condition and the location of your thoracic aortic aneurysm.
- Open-chest surgery. Open-chest surgery to repair a thoracic aortic aneurysm generally involves removing the damaged section of the aorta and replacing it with a synthetic tube (graft), which is sewn into place. It generally takes a month or more to fully recover from this procedure. If you have Marfan syndrome or other related conditions, you may have aortic root replacement. Your surgeon removes a section of your aorta and sometimes the aortic valve and replaces the section of the aorta with a graft. The aortic valve may be replaced with a mechanical or biological valve. If the valve is not removed, the surgery is called valve-sparing aortic root repair.
- Endovascular surgery. Doctors attach a synthetic graft to the end of a thin tube that's inserted through an artery in your leg and threaded up into your aorta. The graft — a woven tube covered by a metal mesh support — is placed at the site of the aneurysm. Small hooks or pins keep the graft in place. The graft reinforces the weakened section of the aorta to prevent rupture of the aneurysm. Recovery time is generally faster with this procedure than with open-chest surgery, but endovascular surgery can't be done on everyone. Ask your doctor whether it's right for you. After endovascular surgery, you'll need to have regular follow-up imaging scans to ensure that the graft isn't leaking.
- Emergency surgery. Although it's possible to repair a ruptured aortic aneurysm with emergency surgery, the risk is much higher and there is a greater chance of complications. Because of this, doctors prefer to identify and treat thoracic aortic aneurysms before they rupture, and to follow through with lifelong monitoring and appropriate preventive surgery.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Thoracic aortic aneurysm and Learn More about Diseases

Claudication

Diphtheria

Giardial Dysentry

Niemann-Pick

Dry socket

Urethral stricture

Pyoderma gangrenosum

Exercise headaches
thoracic aortic aneurysm, থোরাকিক অ্যারটিক অ্যানিউরিজম
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.