 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Postherpetic neuralgia

Postherpetic neuralgia (PHN) is a type of nerve pain that occurs after an individual experiences an outbreak of shingles, which is caused by the varicella-zoster virus, the same virus that causes chickenpox. PHN is caused by damage to the nerves that occurs during the shingles outbreak.
Symptoms of PHN may include a burning or stabbing pain in the area where the shingles outbreak occurred, sensitivity to touch, itching or numbness, and weakness in the affected area. These symptoms can persist for weeks or even months after the shingles outbreak has healed.
Treatment of PHN may involve medication to manage pain, such as topical analgesics, anticonvulsants, and antidepressants. In some cases, nerve blocks or other interventional procedures may be used to provide relief from pain. Additionally, physical therapy, relaxation techniques, and other complementary therapies may be recommended to help manage symptoms and improve quality of life.
Prevention of shingles through vaccination is the most effective way to prevent PHN. Vaccination is recommended for adults over the age of 50, and for individuals who have had chickenpox in the past. Early treatment of shingles outbreaks with antiviral medications can also help reduce the risk of developing PHN.
PHN can be a debilitating condition that can significantly affect quality of life. It is important to seek medical attention if symptoms of PHN are present, as early diagnosis and treatment can help improve outcomes and minimize complications.
Research Papers
Disease Signs and Symptoms
- Sensitivity to light (Photophobia)
- Itching
- Numbness
- Less commonly, postherpetic neuralgia can produce an itchy feeling or numbness.
Disease Causes
Postherpetic neuralgia
Once you've had chickenpox, the virus remains in your body for the rest of your life. As you age or if your immune system is suppressed, such as from medications or chemotherapy, the virus can reactivate, causing shingles.
Postherpetic neuralgia occurs if your nerve fibers are damaged during an outbreak of shingles. Damaged fibers can't send messages from your skin to your brain as they normally do. Instead, the messages become confused and exaggerated, causing chronic, often excruciating pain that can last months — or even years.
Disease Prevents
Postherpetic neuralgia
The Centers for Disease Control and Prevention (CDC) recommends that adults 50 and older get a Shingrix vaccine to prevent shingles, even if they've had shingles or the older vaccine Zostavax. Shingrix is given in two doses, two to six months apart.
The CDC says two doses of Shingrix is more than 90 percent effective in preventing shingles and postherpetic neuralgia. Shingrix is preferred over Zostavax. The effectiveness may be sustained for a longer period of time than Zostavax. Zostavax may still be used sometimes for healthy adults age 60 and older who aren't allergic to Zostavax and who don't take immune-suppressing medications.
Disease Treatments
No single treatment relieves postherpetic neuralgia for everyone. It often takes a combination of treatments to reduce the pain.
Lidocaine skin patches
These are small, bandage-like patches that contain the topical pain-relieving medication lidocaine. These patches can be cut to fit only the affected area. You apply the patches, available by prescription or over-the-counter at a slightly lower dosage, directly to painful skin to deliver temporary relief.
Capsaicin skin patch
A high concentration of an extract of chili peppers (capsaicin) is available as a skin patch (Qutenza) to relieve pain. Available only in your doctor's office, the patch is applied by trained personnel after using a numbing medication on the affected area.
The process takes at least two hours because you need to be monitored after the high-concentration patch is applied, but a single application decreases pain for some people for up to three months. If it works, the application can be repeated every three months.
Anticonvulsants
Certain anti-seizure medications, including gabapentin (Gralise, Horizant, Neurontin) and pregabalin (Lyrica), can lessen the pain of postherpetic neuralgia. These medications stabilize abnormal electrical activity in your nervous system caused by injured nerves. Side effects include drowsiness, unclear thinking, unsteadiness and swelling in the feet.
Antidepressants
Certain antidepressants — such as nortriptyline (Pamelor), amitriptyline, duloxetine (Cymbalta) and venlafaxine (Effexor XR) — affect key brain chemicals that play a role in both depression and how your body interprets pain. Doctors often prescribe antidepressants for postherpetic neuralgia in smaller doses than they do for depression alone.
Common side effects of these medications include drowsiness, dry mouth, lightheadedness and weight gain.
Opioid painkillers
Some people might need prescription-strength pain medications containing tramadol (Ultram, Conzip), oxycodone (Percocet, Roxicet) or morphine. Opioids can cause mild dizziness, drowsiness, confusion and constipation.
However, recent CDC guidelines urge doctors to consider treatments other than opioids for pain that isn't cancer-related, such as the pain of postherpetic neuralgia. This is based on increasing recognition of the risk of addiction and death in some people using opioids.
If prescribed, opioids need to be monitored closely, used at the lowest possible dose and considered only in situations where safer medications have failed.
Opioid medication can impair your ability to drive and should not be combined with alcohol or other drugs.
Steroid injections
Steroids are sometimes injected into the spine (intrathecal or epidural) for postherpetic neuralgia. However, evidence of effectiveness is inconsistent. A low risk of serious side effects, including meningitis, has been associated with their use.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Postherpetic neuralgia and Learn More about Diseases
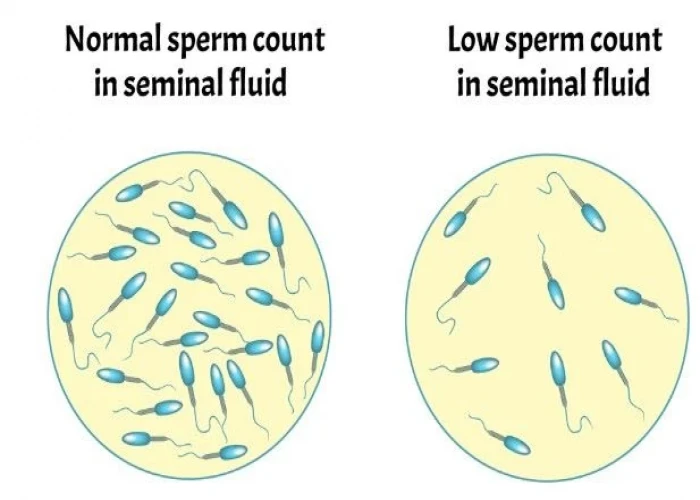
Low sperm count

HIV / AIDS

Ascites
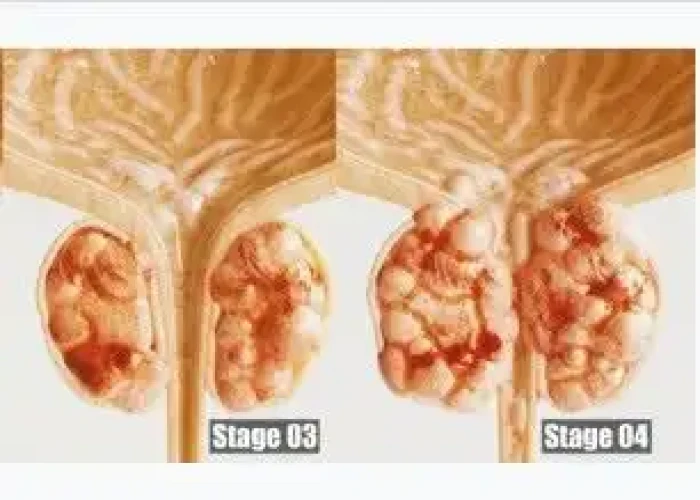
Stage 4 prostate cancer

Muscle strains
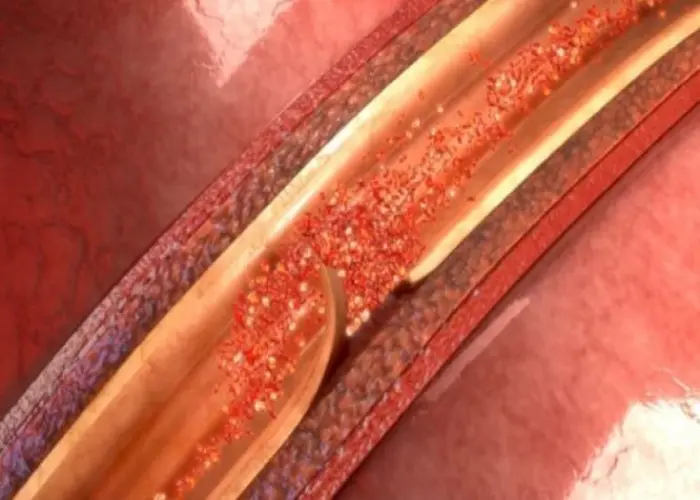
Aortic dissection

Scleroderma
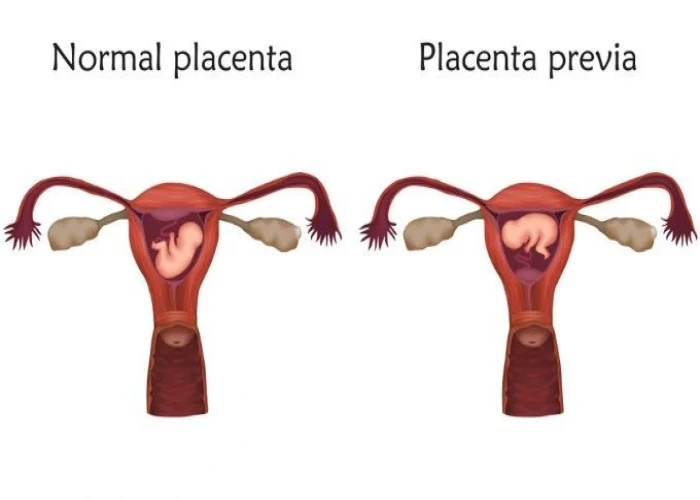
Placenta previa
postherpetic neuralgia, পোস্টেরপেটিক নিউরালজিয়া
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
