 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Stroke

A stroke is a medical emergency that occurs when blood flow to the brain is interrupted, either due to a blood clot or a ruptured blood vessel. Without oxygen and nutrients from the blood, brain cells begin to die, which can lead to permanent brain damage or even death.
The symptoms of a stroke can vary depending on the location and severity of the brain damage, but can include:
- Sudden numbness or weakness in the face, arm, or leg, particularly on one side of the body
- Sudden confusion or trouble speaking or understanding speech
- Sudden trouble seeing in one or both eyes
- Sudden trouble walking, dizziness, or loss of balance or coordination
- Sudden severe headache with no known cause
If you suspect that someone is having a stroke, it is important to call emergency services immediately. Treatment for a stroke typically involves emergency medical care to restore blood flow to the brain and prevent further brain damage. This may involve medications to dissolve blood clots or surgery to repair a ruptured blood vessel.
Recovery from a stroke can be a long and difficult process and may involve rehabilitation to help regain lost function and improve quality of life. This may include physical therapy, speech therapy, occupational therapy, and other treatments as needed. Preventing future strokes may involve managing underlying risk factors such as high blood pressure, high cholesterol, and diabetes, as well as making lifestyle changes such as exercising regularly, eating a healthy diet, and not smoking.
Research Papers
Disease Signs and Symptoms
- Confusion (Hallucinations)
- A sudden, severe headache, which may be accompanied by vomiting, dizziness or altered consciousness, may indicate that having a stroke.
- May experience confusion, slurred words or have difficulty understanding speech.
- Indented streaks or lines on the abdomen, breasts, hips, buttocks or other places on the body
- Poor coordination
- Dizziness (vertigo)
- Dizziness when moving
- Lose balance
- Loss of consciousness (fainting)
- Headaches
- Blurred vision of eye
- Weakness and numbness in legs
- Weakness and numbness in arms
- May also have sudden dizziness or a loss of coordination.
Disease Causes
Stroke
There are two main causes of stroke: a blocked artery (ischemic stroke) or leaking or bursting of a blood vessel (hemorrhagic stroke). Some people may have only a temporary disruption of blood flow to the brain, known as a transient ischemic attack (TIA), that doesn't cause lasting symptoms.
Ischemic stroke
This is the most common type of stroke. It happens when the brain's blood vessels become narrowed or blocked, causing severely reduced blood flow (ischemia). Blocked or narrowed blood vessels are caused by fatty deposits that build up in blood vessels or by blood clots or other debris that travel through the bloodstream, most often from the heart, and lodge in the blood vessels in the brain.
Some initial research shows that COVID-19 infection may increase the risk of ischemic stroke, but more study is needed.
Hemorrhagic stroke
Hemorrhagic stroke occurs when a blood vessel in the brain leaks or ruptures. Brain hemorrhages can result from many conditions that affect the blood vessels. Factors related to hemorrhagic stroke include:
- Uncontrolled high blood pressure
- Overtreatment with blood thinners (anticoagulants)
- Bulges at weak spots in your blood vessel walls (aneurysms)
- Trauma (such as a car accident)
- Protein deposits in blood vessel walls that lead to weakness in the vessel wall (cerebral amyloid angiopathy)
- Ischemic stroke leading to hemorrhage
A less common cause of bleeding in the brain is the rupture of an irregular tangle of thin-walled blood vessels (arteriovenous malformation).
Transient ischemic attack (TIA)
A transient ischemic attack (TIA) — sometimes known as a ministroke — is a temporary period of symptoms similar to those in a stroke. A TIA doesn't cause permanent damage. A TIA is caused by a temporary decrease in blood supply to part of the brain, which may last as little as five minutes.
Like an ischemic stroke, a TIA occurs when a clot or debris reduces or blocks blood flow to part of the nervous system.
Seek emergency care even if you think you've had a TIA because your symptoms got better. It's not possible to tell if you're having a stroke or TIA based only on the symptoms. If you've had a TIA, it means you may have a partially blocked or narrowed artery leading to the brain. Having a TIA increases your risk of having a full-blown stroke later.
Disease Prevents
Stroke
Knowing your stroke risk factors, following your health care provider's recommendations and adopting a healthy lifestyle are the best steps you can take to prevent a stroke. If you've had a stroke or a transient ischemic attack (TIA), these measures might help prevent another stroke. The follow-up care you receive in the hospital and afterward also may play a role.
Many stroke prevention strategies are the same as strategies to prevent heart disease. In general, healthy lifestyle recommendations include:
- Controlling high blood pressure (hypertension). This is one of the most important things you can do to reduce your stroke risk. If you've had a stroke, lowering your blood pressure can help prevent a subsequent TIA or stroke. Healthy lifestyle changes and medications are often used to treat high blood pressure.
- Lowering the amount of cholesterol and saturated fat in your diet. Eating less cholesterol and fat, especially saturated fat and trans fats, may reduce buildup in the arteries. If you can't control your cholesterol through dietary changes alone, your doctor may prescribe a cholesterol-lowering medication.
- Quitting tobacco use. Smoking raises the risk of stroke for smokers and nonsmokers exposed to secondhand smoke. Quitting tobacco use reduces the risk of stroke.
- Managing diabetes. Diet, exercise and losing weight can help you keep your blood sugar in a healthy range. If lifestyle factors don't seem to be enough to control your diabetes, your doctor may prescribe diabetes medication.
- Maintaining a healthy weight. Being overweight contributes to other stroke risk factors, such as high blood pressure, cardiovascular disease and diabetes.
- Eating a diet rich in fruits and vegetables. A diet containing five or more daily servings of fruits or vegetables may reduce the risk of stroke. The Mediterranean diet, which emphasizes olive oil, fruit, nuts, vegetables and whole grains, may be helpful.
- Exercising regularly. Aerobic exercise reduces the risk of stroke in many ways. Exercise can lower blood pressure, increase the levels of good cholesterol, and improve the overall health of the blood vessels and heart. It also helps you lose weight, control diabetes and reduce stress. Gradually work up to at least 30 minutes of moderate physical activity — such as walking, jogging, swimming or bicycling — on most, if not all, days of the week.
- Drinking alcohol in moderation, if at all. Heavy alcohol consumption increases the risk of high blood pressure, ischemic strokes and hemorrhagic strokes. Alcohol may also interact with other drugs you're taking. However, drinking small to moderate amounts of alcohol, such as one drink a day, may help prevent ischemic stroke and decrease the blood's clotting tendency. Talk to your doctor about what's appropriate for you.
- Treating obstructive sleep apnea (OSA). Your doctor may recommend a sleep study if you have symptoms of OSA — a sleep disorder that causes you to stop breathing for short periods repeatedly during sleep. Treatment for OSA includes a device that delivers positive airway pressure through a mask to keep the airway open while you sleep.
- Avoiding illegal drugs. Certain street drugs, such as cocaine and methamphetamine, are established risk factors for a TIA or a stroke.
Preventive medications
If you've had an ischemic stroke or a TIA, your doctor may recommend medications to help reduce your risk of having another stroke. These include:
- Anti-platelet drugs. Platelets are cells in the blood that form clots. Anti-platelet drugs make these cells less sticky and less likely to clot. The most commonly used anti-platelet medication is aspirin. Your doctor can help you determine the right dose of aspirin for you.
- After a TIA or minor stroke, your doctor may give you aspirin and an anti-platelet drug such as clopidogrel (Plavix) for a period of time to reduce the risk of another stroke. If you can't take aspirin, your doctor may prescribe clopidogrel alone.
- Anticoagulants. These drugs reduce blood clotting. Heparin is fast acting and may be used short-term in the hospital.
- Slower-acting warfarin (Jantoven) may be used over a longer term. Warfarin is a powerful blood-thinning drug, so you'll need to take it exactly as directed and watch for side effects. You'll also need to have regular blood tests to monitor warfarin's effects.
- Several newer blood-thinning medications (anticoagulants) are available for preventing strokes in people who have a high risk. These medications include dabigatran (Pradaxa), rivaroxaban (Xarelto), apixaban (Eliquis) and edoxaban (Savaysa). They're shorter acting than warfarin and usually don't require regular blood tests or monitoring by your doctor. These drugs are also associated with a lower risk of bleeding complications compared to warfarin.
Disease Treatments
Emergency treatment for stroke depends on whether you're having an ischemic stroke or a stroke that involves bleeding into the brain (hemorrhagic).
Ischemic stroke
To treat an ischemic stroke, doctors must quickly restore blood flow to the brain. This may be done with:
- Emergency IV medication. Therapy with drugs that can break up a clot has to be given within 4.5 hours from when symptoms first started if given intravenously. The sooner these drugs are given, the better. Quick treatment not only improves your chances of survival but also may reduce complications.
- An IV injection of recombinant tissue plasminogen activator (TPA) — also called alteplase (Activase) or tenecteplase (TNKase) — is the gold standard treatment for ischemic stroke. An injection of TPA is usually given through a vein in the arm within the first three hours. Sometimes, TPA can be given up to 4.5 hours after stroke symptoms started.
- This drug restores blood flow by dissolving the blood clot causing the stroke. By quickly removing the cause of the stroke, it may help people recover more fully from a stroke. Your doctor will consider certain risks, such as potential bleeding in the brain, to determine whether TPA is appropriate for you.
- Emergency endovascular procedures. Doctors sometimes treat ischemic strokes directly inside the blocked blood vessel. Endovascular therapy has been shown to significantly improve outcomes and reduce long-term disability after ischemic stroke. These procedures must be performed as soon as possible:
- Medications delivered directly to the brain. Doctors insert a long, thin tube (catheter) through an artery in the groin and thread it to the brain to deliver TPA directly where the stroke is happening. The time window for this treatment is somewhat longer than for injected TPA but is still limited.
- Removing the clot with a stent retriever. Doctors can use a device attached to a catheter to directly remove the clot from the blocked blood vessel in the brain. This procedure is particularly beneficial for people with large clots that can't be completely dissolved with TPA. This procedure is often performed in combination with injected TPA.
The time window when these procedures can be considered has been expanding due to newer imaging technology. Doctors may order perfusion imaging tests (done with CT or MRI) to help determine how likely it is that someone can benefit from endovascular therapy.
Other procedures
To decrease your risk of having another stroke or transient ischemic attack, your doctor may recommend a procedure to open up an artery that's narrowed by plaque. Options vary depending on the situation, but include:
- Carotid endarterectomy. Carotid arteries are the blood vessels that run along each side of the neck, supplying the brain (carotid arteries) with blood. This surgery removes the plaque blocking a carotid artery and may reduce the risk of ischemic stroke. A carotid endarterectomy also involves risks, especially for people with heart disease or other medical conditions.
- Angioplasty and stents. In an angioplasty, a surgeon threads a catheter to the carotid arteries through an artery in the groin. A balloon is then inflated to expand the narrowed artery. Then a stent can be inserted to support the opened artery.
Hemorrhagic stroke
Emergency treatment of hemorrhagic stroke focuses on controlling the bleeding and reducing pressure in the brain caused by the excess fluid. Treatment options include:
- Emergency measures. If you take blood-thinning medications to prevent blood clots, you may be given drugs or transfusions of blood products to counteract the blood thinners' effects. You may also be given drugs to lower the pressure in the brain (intracranial pressure), lower blood pressure, prevent spasms of the blood vessels and prevent seizures.
- Surgery. If the area of bleeding is large, your doctor may perform surgery to remove the blood and relieve pressure on the brain. Surgery may also be used to repair blood vessel problems associated with hemorrhagic strokes. Your doctor may recommend one of these procedures after a stroke or if an aneurysm, arteriovenous malformation (AVM) or other type of blood vessel problem caused the hemorrhagic stroke.
- Surgical clipping. A surgeon places a tiny clamp at the base of the aneurysm to stop blood flow to it. This clamp can keep the aneurysm from bursting, or it can keep an aneurysm that has recently hemorrhaged from bleeding again.
- Coiling (endovascular embolization). Using a catheter inserted into an artery in the groin and guided to the brain, the surgeon will place tiny detachable coils into the aneurysm to fill it. This blocks blood flow into the aneurysm and causes blood to clot.
- Surgical AVM removal. Surgeons may remove a smaller AVM if it's located in an accessible area of the brain. This eliminates the risk of rupture and lowers the risk of hemorrhagic stroke. However, it's not always possible to remove an AVM if it's located deep within the brain, it's large, or its removal would cause too much of an impact on brain function.
- Stereotactic radiosurgery. Using multiple beams of highly focused radiation, stereotactic radiosurgery is an advanced minimally invasive treatment used to repair blood vessel malformations.
Stroke recovery and rehabilitation
After emergency treatment, you'll be closely monitored for at least a day. After that, stroke care focuses on helping you recover as much function as possible and return to independent living. The impact of the stroke depends on the area of the brain involved and the amount of tissue damaged.
If the stroke affected the right side of the brain, your movement and sensation on the left side of the body may be affected. If the stroke damaged the brain tissue on the left side of the brain, your movement and sensation on the right side of the body may be affected. Brain damage to the left side of the brain may cause speech and language disorders.
Most stroke survivors go to a rehabilitation program. Your doctor will recommend the most rigorous therapy program you can handle based on your age, overall health and degree of disability from the stroke. Your doctor will take into consideration your lifestyle, interests and priorities, and the availability of family members or other caregivers.
Rehabilitation may begin before you leave the hospital. After discharge, you might continue your program in a rehabilitation unit of the same hospital, another rehabilitation unit or skilled nursing facility, as an outpatient, or at home.
Every person's stroke recovery is different. Depending on your condition, your treatment team may include:
- Doctor trained in brain conditions (neurologist)
- Rehabilitation doctor (physiatrist)
- Rehabilitation nurse
- Dietitian
- Physical therapist
- Occupational therapist
- Recreational therapist
- Speech pathologist
- Social worker or case manager
- Psychologist or psychiatrist
- Chaplain
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Stroke and Learn More about Diseases

Body dysmorphic disorder

Microscopic colitis

Periodontitis (Pyrrhoea)
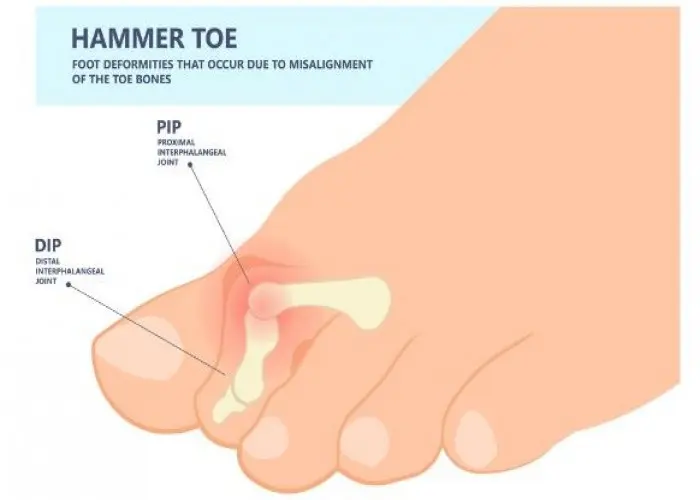
Hammertoe and mallet toe

Thyroid nodules

Osteochondritis dissecans

Pink eye (conjunctivitis)
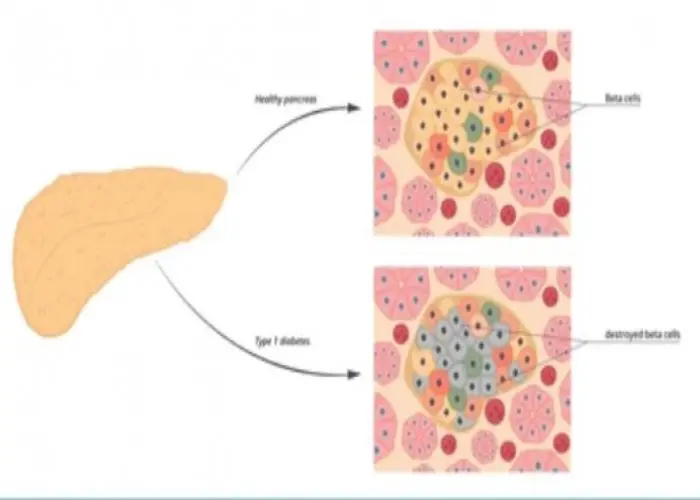
Autoimmune pancreatitis
stroke, স্ট্রোক
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
