 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Psoriatic arthritis

Psoriatic arthritis is a type of arthritis that can develop in people with psoriasis, a chronic skin condition characterized by scaly and itchy patches on the skin. Psoriatic arthritis is thought to be an autoimmune disorder, which means that the body's immune system mistakenly attacks healthy tissues and joints, leading to inflammation and joint damage.
The symptoms of psoriatic arthritis can vary in severity and can affect any joint in the body, including the fingers, toes, spine, and pelvis. Common symptoms include joint pain, stiffness, and swelling, as well as fatigue, nail changes, and the development of new or worsening psoriasis.
Diagnosis of psoriatic arthritis typically involves a combination of a physical examination, medical history, blood tests, and imaging studies such as X-rays or magnetic resonance imaging (MRI) scans. The diagnosis may be challenging, as the symptoms of psoriatic arthritis can be similar to those of other types of arthritis.
Treatment for psoriatic arthritis typically involves a combination of medications, lifestyle changes, and physical therapy. Medications may include nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce pain and inflammation, disease-modifying antirheumatic drugs (DMARDs) to slow the progression of the disease, and biologic medications that target specific parts of the immune system. Lifestyle changes may include exercise, weight management, stress reduction, and avoiding triggers such as smoking and alcohol.
While there is no cure for psoriatic arthritis, with proper treatment and management, most people with the condition are able to manage their symptoms and maintain their quality of life. It is important to work with a healthcare professional to develop an individualized treatment plan that takes into account the severity and location of the symptoms, as well as the person's overall health and lifestyle.
Research Papers
Disease Signs and Symptoms
- Swollen toe
- Swollen fingers
- Foot pain
- Lower back pain
- Eye pain or burning
- Developed swelling and deformities in hands and feet before having significant joint symptoms.
Disease Causes
Psoriatic arthritis
Psoriatic arthritis occurs when your body's immune system attacks healthy cells and tissue. The immune response causes inflammation in your joints as well as overproduction of skin cells.
It seems likely that both genetic and environmental factors play a role in this immune system response. Many people with psoriatic arthritis have a family history of either psoriasis or psoriatic arthritis. Researchers have discovered certain genetic markers that appear to be associated with psoriatic arthritis.
Physical trauma or something in the environment — such as a viral or bacterial infection — might trigger psoriatic arthritis in people with an inherited tendency.
Disease Prevents
Disease Treatments
No cure exists for psoriatic arthritis. Treatment focuses on controlling inflammation in your affected joints to prevent joint pain and disability and controlling skin involvement. One of the most common treatments are prescription medications called disease-modifying antirheumatic drugs (DMARDs).
Treatment will depend on how severe your disease is and what joints are affected. You might have to try different treatments before you find one that brings you relief.
Medications
Drugs used to treat psoriatic arthritis include:
- NSAIDs. Nonsteroidal anti-inflammatory drugs (NSAIDs) can relieve pain and reduce inflammation for people with mild psoriatic arthritis. NSAIDs available without a prescription include ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve). Stronger NSAIDs are available by prescription. Side effects can include stomach irritation, heart problems, and liver and kidney damage.
- Conventional DMARDs. These drugs can slow the progression of psoriatic arthritis and save joints and other tissues from permanent damage.
- The most commonly used DMARD is methotrexate (Trexall, Otrexup, others). Others include leflunomide (Arava) and sulfasalazine (Azulfidine). Side effects can include liver damage, bone marrow suppression, and lung inflammation and scarring (fibrosis).
- Biologic agents. Also known as biologic response modifiers, this class of DMARD targets different pathways of the immune system. Biologic agents include adalimumab (Humira), certolizumab (Cimzia), etanercept (Enbrel), golimumab (Simponi), infliximab (Remicade), ustekinumab (Stelara), secukinumab (Cosentyx), ixekizumab (Taltz), guselkumab (Tremfya) and abatacept (Orencia). These drugs can increase the risk of infections.
- Targeted synthetic DMARDs. Tofacitinib (Xeljanz) might be used if conventional DMARDs and biologic agents haven't been effective. Higher doses of tofacitinib can increase the risk of blood clots in the lungs, serious heart-related events and cancer.
- Newer oral medication. Apremilast (Otezla) decreases the activity of an enzyme in the body that controls the activity of inflammation within cells. Apremilast is used for people with mild to moderate psoriatic arthritis who do not want or cannot be treated with DMARDs or biologic agents. Potential side effects include diarrhea, nausea and headaches.
Therapies
Physical and occupational therapies might ease pain and make it easier to do everyday tasks. Ask your doctor for referrals. Massage therapy might also offer relief.
Surgical and other procedures
- Steroid injections. Injections into an affected joint can reduce inflammation.
- Joint replacement surgery. Some joints that have been severely damaged by psoriatic arthritis can be replaced with artificial ones made of metal and plastic.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Psoriatic arthritis and Learn More about Diseases

Jet lag disorder
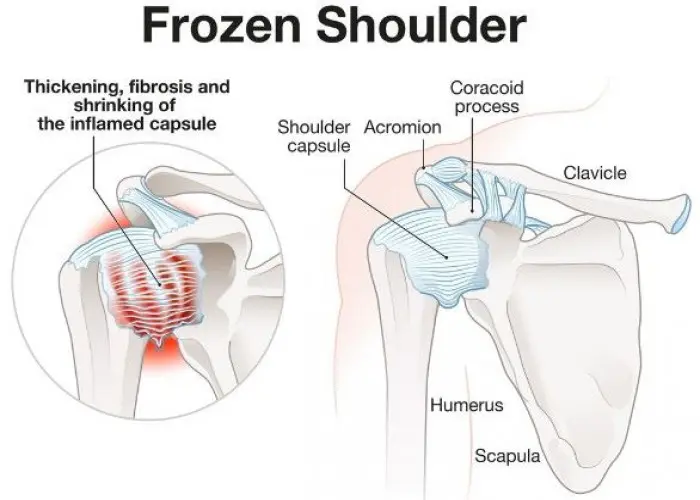
Frozen shoulder

Marfan syndrome

Vaginal cancer
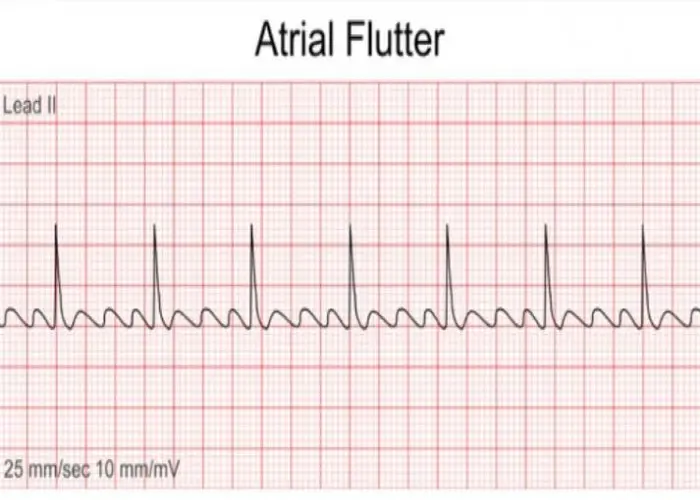
Atrial flutter

Amyotrophic lateral sclerosis (ALS)

Diabetic nephropathy
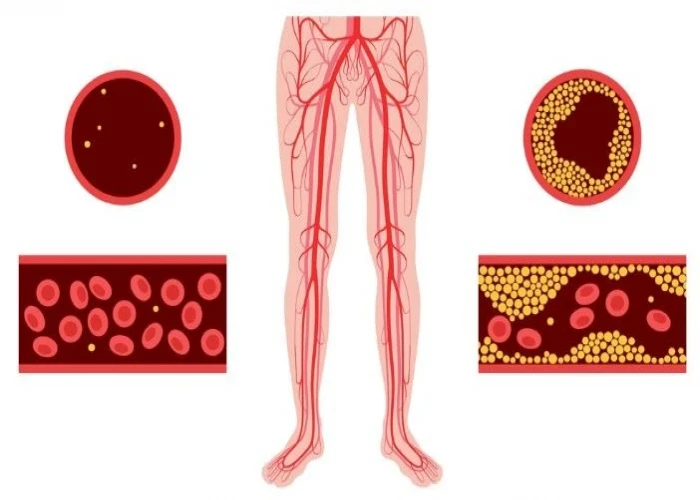
Peripheral artery disease (PAD)
psoriatic arthritis, পসোরিয়াটিক বাত
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
