Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
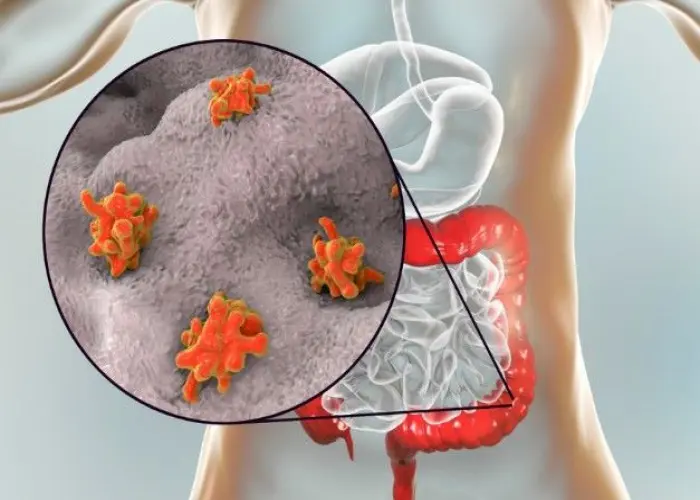
Fecal incontinence
Fecal incontinence is the inability to control bowel movements, leading to involuntary loss of stool (feces) or gas. It can be a very distressing condition that affects the quality of life, self-esteem, and social functioning.
Fecal incontinence can have various causes, including damage to the nerves or muscles that control bowel movements, certain medical conditions such as inflammatory bowel disease or diabetes, pelvic floor dysfunction, or injury to the anal sphincter muscles. It can also be a side effect of certain medications, such as laxatives or antibiotics.
Treatment for fecal incontinence depends on the underlying cause, the severity of the condition, and individual circumstances. It may involve dietary changes, medications, biofeedback, pelvic floor muscle exercises, surgery, or the use of bowel management systems. A healthcare professional, such as a gastroenterologist, colorectal surgeon, or urogynecologist, can help diagnose the underlying cause and recommend appropriate treatment options.
Research Papers
Disease Signs and Symptoms
- Diarrhea
- Constipation
- Gas
- Abdomen bloating
Disease Causes
Fecal incontinence
For many people, there is more than one cause of fecal incontinence.
Causes can include:
- Muscle damage. Injury to the rings of muscle at the end of the rectum (anal sphincter) may make it difficult to hold stool back properly. This kind of damage can occur during childbirth, especially if you have an episiotomy or forceps are used during delivery.
- Nerve damage. Injury to the nerves that sense stool in the rectum or those that control the anal sphincter can lead to fecal incontinence. The nerve damage can be caused by childbirth, constant straining during bowel movements, spinal cord injury or a stroke. Some diseases, such as diabetes and multiple sclerosis, also can affect these nerves and cause damage that leads to fecal incontinence.
- Constipation. Chronic constipation may cause a dry, hard mass of stool (impacted stool) to form in the rectum and become too large to pass. The muscles of the rectum and intestines stretch and eventually weaken, allowing watery stool from farther up the digestive tract to move around the impacted stool and leak out. Chronic constipation may also cause nerve damage that leads to fecal incontinence.
- Diarrhea. Solid stool is easier to retain in the rectum than is loose stool, so the loose stools of diarrhea can cause or worsen fecal incontinence.
- Hemorrhoids. When the veins in your rectum swell, causing hemorrhoids, this keeps your anus from closing completely, which can allow stool to leak out.
- Loss of storage capacity in the rectum. Normally, the rectum stretches to accommodate stool. If your rectum is scarred or stiff due to surgery, radiation treatment or inflammatory bowel disease, the rectum can't stretch as much as it needs to, and excess stool can leak out.
- Surgery. Surgery to treat enlarged veins in the rectum or anus (hemorrhoids), as well as more-complex operations involving the rectum and anus, can cause muscle and nerve damage that leads to fecal incontinence.
- Rectal prolapse. Fecal incontinence can be a result of this condition, in which the rectum drops down into the anus. The stretching of the rectal sphincter by prolapse damages the nerves that control the rectal sphincter. The longer this persists, the less likely the nerves and muscles will recover.
- Rectocele. In women, fecal incontinence can occur if the rectum protrudes through the vagina.
Disease Prevents
Fecal incontinence
Depending on the cause, it may be possible to improve or prevent fecal incontinence. These actions may help:
- Reduce constipation. Increase your exercise, eat more high-fiber foods and drink plenty of fluids.
- Control diarrhea. Treating or eliminating the cause of the diarrhea, such as an intestinal infection, may help you avoid fecal incontinence.
- Avoid straining. Straining during bowel movements can eventually weaken anal sphincter muscles or damage nerves, possibly leading to fecal incontinence.
Disease Treatments
Medications
Depending on the cause of fecal incontinence, options include:
- Anti-diarrheal drugs such as loperamide hydrochloride (Imodium A-D) and diphenoxylate and atropine sulfate (Lomotil)
- Bulk laxatives such as methylcellulose (Citrucel) and psyllium (Metamucil), if chronic constipation is causing your incontinence
Exercise and other therapies
If muscle damage is causing fecal incontinence, your doctor may recommend a program of exercise and other therapies to restore muscle strength. These treatments can improve anal sphincter control and the awareness of the urge to defecate.
Options include:
- Kegel exercises. Kegel exercises strengthen the pelvic floor muscles, which support the bladder and bowel and, in women, the uterus, and may help reduce incontinence. To perform Kegel exercises, contract the muscles that you would normally use to stop the flow of urine.
- Hold the contraction for three seconds, then relax for three seconds. Repeat this pattern 10 times. As your muscles strengthen, hold the contraction longer, gradually working your way up to three sets of 10 contractions every day.
- Biofeedback. Specially trained physical therapists teach simple exercises that can increase anal muscle strength. People learn how to strengthen pelvic floor muscles, sense when stool is ready to be released and contract the muscles if having a bowel movement at a certain time is inconvenient. Sometimes the training is done with the help of anal manometry and a rectal balloon.
- Bowel training. Your doctor may recommend making a conscious effort to have a bowel movement at a specific time of day: for example, after eating. Establishing when you need to use the toilet can help you gain greater control.
- Bulking agents. Injections of nonabsorbable bulking agents can thicken the walls of your anus. This helps prevent leakage.
- Sacral nerve stimulation (SNS). The sacral nerves run from your spinal cord to muscles in your pelvis, and regulate the sensation and strength of your rectal and anal sphincter muscles. Implanting a device that sends small electrical impulses continuously to the nerves can strengthen muscles in the bowel.
- Posterior tibial nerve stimulation (PTNS/TENS). This minimally invasive treatment stimulates the posterior tibial nerve at the ankle. In a large study, however, this therapy didn't prove to be significantly better than a placebo.
- Vaginal balloon (Eclipse System). This is a pump-type device inserted in the vagina. The inflated balloon results in pressure on the rectal area, leading to a decrease in the number of episodes of fecal incontinence.
- Radiofrequency therapy. Known as the Secca procedure, this involves delivering temperature-controlled radiofrequency energy to the wall of the anal canal to help improve muscle tone. Radiofrequency therapy is minimally invasive and is generally performed under local anesthesia and sedation. However, this procedure isn't always covered by insurance.
Surgery
Treating fecal incontinence may require surgery to correct an underlying problem, such as rectal prolapse or sphincter damage caused by childbirth. The options include:
- Sphincteroplasty. This procedure repairs a damaged or weakened anal sphincter that occurred during childbirth. Doctors identify an injured area of muscle and free its edges from the surrounding tissue. They then bring the muscle edges back together and sew them in an overlapping fashion, strengthening the muscle and tightening the sphincter. Sphincteroplasty may be an option for patients trying to avoid colostomy.
- Treating rectal prolapse, a rectocele or hemorrhoids. Surgical correction of these problems will likely reduce or eliminate fecal incontinence. Over time, the prolapse of the rectum through the rectal sphincter damages the nerves and muscles of the sphincter. The longer the prolapse goes untreated, the higher will be the risk of fecal incontinence not resolving after surgery.
- Colostomy (bowel diversion). This surgery diverts stool through an opening in the abdomen. Doctors attach a special bag to this opening to collect the stool. Colostomy is generally considered only after other treatments haven't been successful.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Fecal incontinence and Learn More about Diseases

Pulmonary atresia

Progressive supranuclear palsy

Rectal prolapse
Aortic valve regurgitation
Heart disease

Botulism
Amoebic Dysentry

Rocky Mountain spotted fever
fecal incontinence, মলত্যাগের অনিয়ম
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.