Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
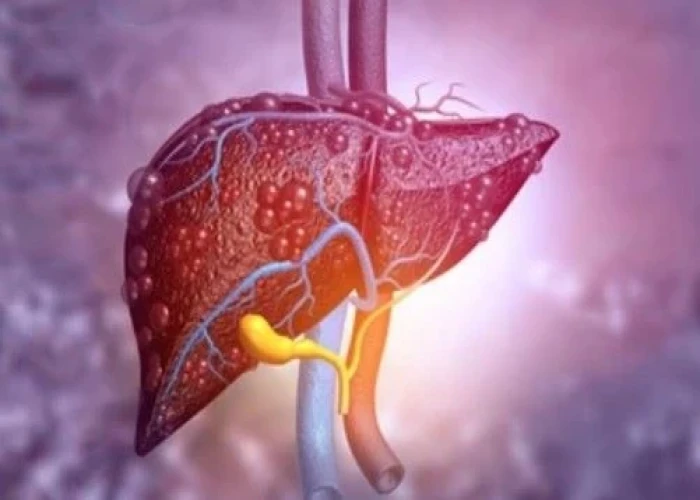
Primary sclerosing cholangitis
Primary sclerosing cholangitis (PSC) is a rare chronic liver disease that affects the bile ducts inside and outside the liver. In PSC, the bile ducts become inflamed and scarred, causing obstruction of the bile flow and damage to the liver cells.
The exact cause of PSC is unknown, but it is believed to be related to a combination of genetic, immune, and environmental factors. PSC is often associated with other autoimmune diseases, such as inflammatory bowel disease (IBD), and is more common in males than females.
The symptoms of PSC can vary widely from person to person and may include fatigue, abdominal pain, itching, jaundice (yellowing of the skin and eyes), and weight loss. Some people with PSC may have no symptoms at all, and the condition may only be discovered during routine blood tests.
The diagnosis of PSC is typically made through a combination of blood tests, imaging studies such as magnetic resonance cholangiopancreatography (MRCP) or endoscopic retrograde cholangiopancreatography (ERCP), and a liver biopsy.
There is no cure for PSC, and treatment is aimed at managing symptoms and preventing complications. Ursodeoxycholic acid (UDCA) may be prescribed to improve bile flow and reduce liver inflammation. Antibiotics may also be prescribed to prevent infections, as people with PSC are at an increased risk of developing infections due to the obstruction of the bile ducts. In severe cases, a liver transplant may be necessary.
People with PSC require regular monitoring and follow-up care to manage their condition and prevent complications such as liver failure or bile duct cancer.
Research Papers
Disease Signs and Symptoms
- Fatigue (Tiredness)
- Swollen spleen (splenomegaly)
- Enlarged liver and spleen
- Night sweats
- Fever and chills
- Fever
- Abdomen pain
- Yellowing of skin and eyes (jaundice)
- Itching
- Weight loss
Disease Causes
Primary sclerosing cholangitis
It's not clear what causes primary sclerosing cholangitis. An immune system reaction to an infection or toxin may trigger the disease in people who are genetically predisposed to it.
A large proportion of people with primary sclerosing cholangitis also have inflammatory bowel disease, an umbrella term that includes ulcerative colitis and Crohn's disease.
Primary sclerosing cholangitis and inflammatory bowel disease don't always appear at the same time, though. In some cases, primary sclerosing cholangitis is present for years before inflammatory bowel disease occurs. If primary sclerosing cholangitis is diagnosed, it's important to look for inflammatory bowel disease because there is a greater risk of colon cancer.
Somewhat less often, people being treated for inflammatory bowel disease turn out to have primary sclerosing cholangitis as well. And rarely, people with primary sclerosing cholangitis develop inflammatory bowel disease only after having a liver transplant.
Disease Prevents
Disease Treatments
Treatments for primary sclerosing cholangitis focus on managing complications and monitoring liver damage. Many medications have been studied in people with primary sclerosing cholangitis, but so far none have been found to slow or reverse the liver damage associated with this disease.
Treatment for itching
- Bile acid sequestrants. Medications that bind to bile acids — the substances thought to cause itching in liver disease — are the first line treatment for itching in primary sclerosing cholangitis.
- Antibiotics. If you have trouble tolerating a bile acid-binding drug or if it doesn't help, your doctor may prescribe rifampin (Rifadin, Rimactane, others), an antibacterial drug. Exactly how rifampin reduces itching is unknown, but it may block the brain's response to itch-inducing chemicals in your circulation.
- Antihistamines. This type of medication may help reduce mild itching caused by primary sclerosing cholangitis. Whether these medications are effective for this condition is unknown.
- Antihistamines may worsen the liver disease symptoms of dry eyes and dry mouth. On the other hand, antihistamines can help with sleep if itching keeps you awake.
- Opioid antagonists. Itching related to liver disease may also respond to opioid antagonist drugs, such as naltrexone. Like rifampin, these drugs seem to reduce the itch sensation by acting on your brain.
- Ursodeoxycholic acid (UDCA). Also known as ursodiol, UDCA is a naturally occurring bile acid that may help relieve itching symptoms caused by liver disease by increasing the absorbability of bile.
Treatment for infections
Bile that backs up in narrowed or blocked ducts causes frequent bacterial infections. To prevent and treat these infections, people with primary sclerosing cholangitis may take repeated courses of antibiotics or continue taking antibiotics for long periods.
Before any procedure that could cause an infection, such as an endoscopic procedure or abdominal surgery, you'll also need to take antibiotics.
Nutrition support
Primary sclerosing cholangitis makes it difficult for your body to absorb certain vitamins. Even though you may eat a healthy diet, you may find that you can't get all the nutrients you need.
Your doctor may recommend vitamin supplements that you take as tablets or that you receive as an infusion through a vein in your arm. If the disease weakens your bones, you may take calcium and vitamin D supplements as well.
Treatment for bile duct blockages
Blockages that occur in your bile ducts may be due to disease progression but can be a sign of cancer of the bile duct. Endoscopic retrograde cholangiopancreatography (ERCP) can help determine the cause, and bile duct blockage can be treated with:
- Balloon dilation. This procedure can open blockages in the larger bile ducts outside the liver. In balloon dilation, your doctor runs a slender tube with an inflatable balloon at its tip (balloon catheter) through an endoscope and into a blocked bile duct. Once the balloon catheter is in place, the balloon is inflated.
- Stent placement. In this procedure, your doctor uses an endoscope and attached instruments to place a small plastic tube called a stent in a blocked bile duct to hold the duct open.
Liver transplant
A liver transplant is the only treatment known to cure primary sclerosing cholangitis. During a liver transplant, surgeons remove your diseased liver and replace it with a healthy liver from a donor.
A liver transplant is reserved for people with liver failure or other severe complications of primary sclerosing cholangitis. Though uncommon, it's possible for primary sclerosing cholangitis to recur after a liver transplant.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Primary sclerosing cholangitis and Learn More about Diseases

Carpal tunnel syndrome
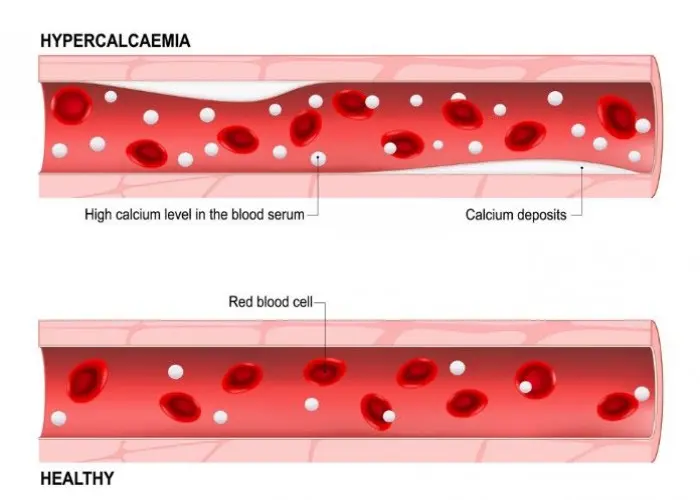
Hypercalcemia
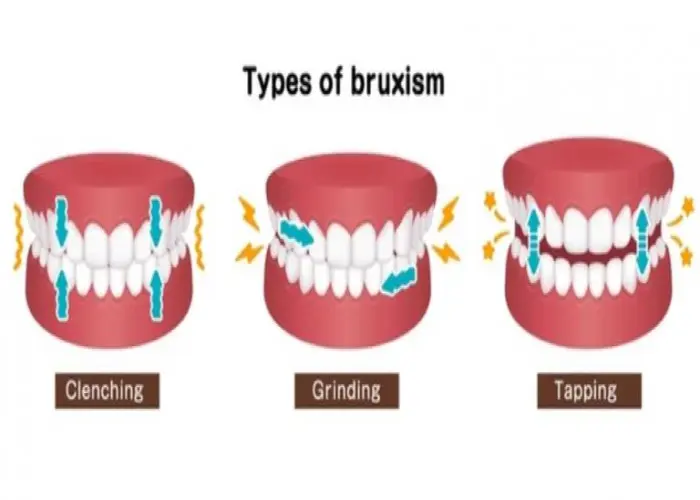
Bruxism (teeth grinding)
Precocious puberty

Glioma

Amyloidosis
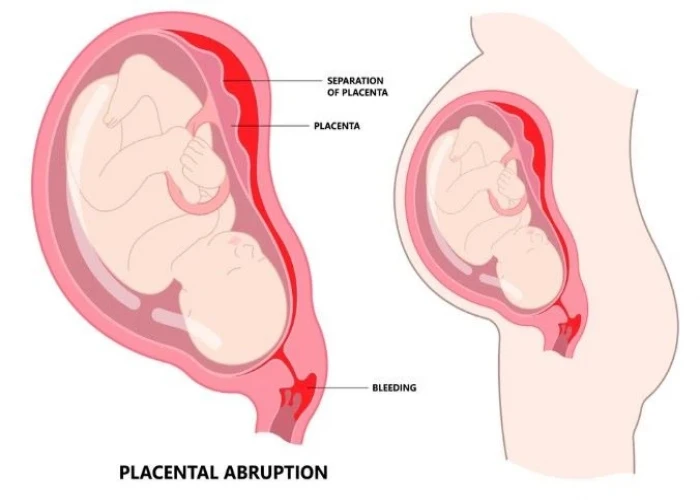
Placental abruption
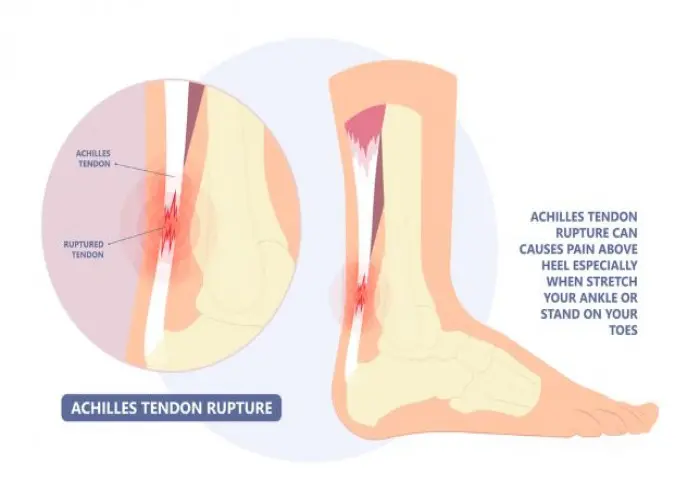
Achilles tendon rupture
primary sclerosing cholangitis, প্রাথমিক স্ক্লেরোসিং কোলেঞ্জাইটিস
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.