Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Esophagitis
Esophagitis is a medical condition characterized by inflammation or irritation of the lining of the esophagus, which is the muscular tube that connects the throat to the stomach. This condition can occur due to a variety of causes, including:
- Acid reflux: When stomach acid flows back into the esophagus, it can irritate and inflame the lining of the esophagus.
- Infections: Certain viral, bacterial, and fungal infections can cause esophagitis.
- Medications: Some medications, such as antibiotics, painkillers, and bisphosphonates, can cause esophagitis if they irritate the lining of the esophagus.
- Allergies: Esophagitis can also occur as a result of an allergic reaction to certain foods, such as milk, soy, and wheat.
Symptoms of esophagitis can include difficulty swallowing, pain or discomfort when swallowing, chest pain, heartburn, and regurgitation of food or sour liquid. Treatment for esophagitis depends on the underlying cause and may include medications to reduce inflammation and control acid reflux, dietary changes, and lifestyle modifications. In severe cases, surgery may be necessary to repair damage to the esophagus.
Research Papers
Disease Signs and Symptoms
- Difficulty swallowing (dysphagia)
- Chest pain
- A painful, burning sensation behind the breastbone
- Swallowed food becoming stuck in the esophagus (food impaction)
- Heartburn
- Acid regurgitation
Disease Causes
Esophagitis
Esophagitis is generally categorized by the conditions that cause it. In some cases, more than one factor may be causing esophagitis.
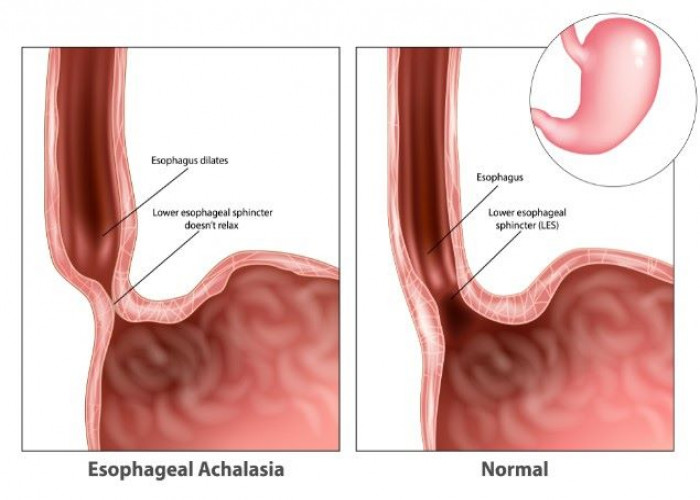
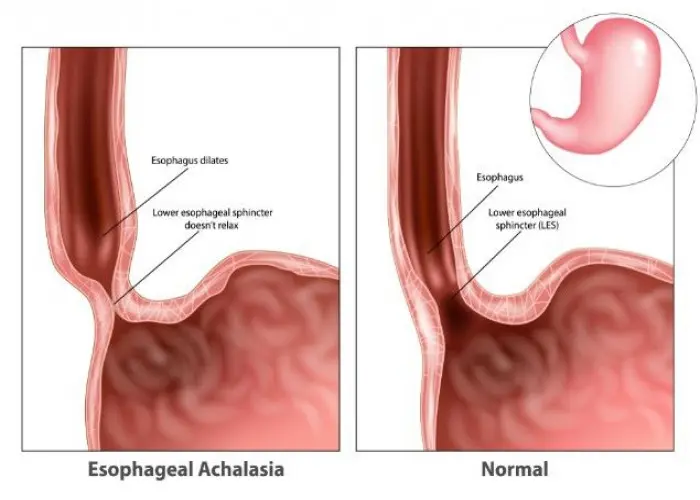
Reflux esophagitis
A valve-like structure called the lower esophageal sphincter usually keeps the acidic contents of the stomach out of the esophagus. If this valve opens when it shouldn't or doesn't close properly, the contents of the stomach may back up into the esophagus (gastroesophageal reflux). Gastroesophageal reflux disease (GERD) is a condition in which this backflow of acid is a frequent or ongoing problem. A complication of GERD is chronic inflammation and tissue damage in the esophagus.
Eosinophilic esophagitis
Eosinophils (e-o-SIN-o-fils) are white blood cells that play a key role in allergic reactions. Eosinophilic esophagitis occurs with a high concentration of these white blood cells in the esophagus, most likely in response to an allergy-causing agent (allergen) or acid reflux or both.
In many cases, this type of esophagitis may be triggered by foods such as milk, eggs, wheat, soy, peanuts, beans, rye and beef. However, conventional allergy testing does not reliably identify these culprit foods.
People with eosinophilic esophagitis may have other nonfood allergies. For example, sometimes inhaled allergens, such as pollen, may be the cause.
Lymphocytic esophagitis
Lymphocytic esophagitis (LE) is an uncommon esophageal condition in which there are an increased number of lymphocytes in the lining of the esophagus. LE may be related to eosinophilic esophagitis or to GERD.
Drug-induced esophagitis
Several oral medications may cause tissue damage if they remain in contact with the lining of the esophagus for too long. For example, if you swallow a pill with little or no water, the pill itself or residue from the pill may remain in the esophagus. Drugs that have been linked to esophagitis include:
- Pain-relieving medications, such as aspirin, ibuprofen (Advil, Motrin, others) and naproxen sodium (Aleve, others)
- Antibiotics, such as tetracycline and doxycycline
- Potassium chloride, which is used to treat potassium deficiency
- Bisphosphonates, including alendronate (Fosamax), a treatment for weak and brittle bones (osteoporosis)
- Quinidine, which is used to treat heart problems
Infectious esophagitis
A bacterial, viral or fungal infection in tissues of the esophagus may cause esophagitis. Infectious esophagitis is relatively rare and occurs most often in people with poor immune system function, such as people with HIV/AIDS or cancer.
A fungus normally present in the mouth called Candida albicans is a common cause of infectious esophagitis. Such infections are often associated with poor immune system function, diabetes, cancer, or the use of steroid or antibiotic medications.
Disease Prevents
Disease Treatments
Treatments for esophagitis are intended to lessen symptoms, manage complications and treat underlying causes of the disorder. Treatment strategies vary primarily based on the cause of the disorder.
Reflux esophagitis
Treatment for reflux esophagitis may include:
- Over-the-counter treatments. These include antacids (Maalox, Mylanta, others); medications that reduce acid production, called H-2-receptor blockers, such as cimetidine (Tagamet HB); and medications that block acid production and heal the esophagus, called proton pump inhibitors, such as lansoprazole (Prevacid) and omeprazole (Prilosec).
- Prescription-strength medications. These include H-2-receptor blockers as well as proton pump inhibitors, such as esomeprazole (Nexium), lansoprazole (Prevacid), omeprazole (Prilosec) and pantoprazole (Protonix). You also may be prescribed prokinetics such as bethanechol and metoclopramide (Reglan), which help your stomach empty more quickly.
- Surgery. Fundoplication may be used to improve the condition of the esophagus if other interventions don't work. A portion of the stomach is wrapped around the valve separating the esophagus and stomach (lower esophageal sphincter). This strengthens the sphincter and prevents acid from backing up into the esophagus.
- A newer treatment involves minimally invasive surgery to place a ring of tiny magnetic titanium beads around the junction of the stomach and esophagus. In that position, the ring of beads strengthens the lower esophageal sphincter, preventing acid reflux.
Eosinophilic esophagitis
Treatment for eosinophilic esophagitis is primarily avoiding the allergen and reducing the allergic reaction with medications. Medications may include:
- Proton pump inhibitors. Your doctor will likely first prescribe a proton pump inhibitor, such as esomeprazole (Nexium), lansoprazole (Prevacid), omeprazole (Prilosec) or pantoprazole (Protonix).
- Steroids. Some studies have shown that swallowed steroids such as fluticasone (Flovent) and budesonide (Pulmicort) may act topically in the esophagus and help treat eosinophilic esophagitis. The same steroid medications that are inhaled to manage asthma are swallowed to treat eosinophilic esophagitis.
- Your doctor will instruct you on how to swallow the steroid preparation so that it coats your esophagus. This delivery system of steroids is much less likely to cause serious side effects than taking oral steroid pills.
- Elimination and elemental diets. A response to a food allergen is likely the cause of eosinophilic esophagitis. Therefore, elimination of the culprit food may be an effective treatment strategy.
- However, as no tests are currently available to identify the culprit food, your doctor may recommend that you remove common food allergens from your diet. Under your doctor's direction, you'll gradually add foods back into your diet and note when symptoms return.
- Another, more restrictive, approach is to remove all food from your diet and replace it with an amino acid-based formula.
New biologic therapies are being developed to treat eosinophilic esophagitis and will likely be available within a few years. These medications stimulate your body's immune response to fight infection, inflammation or disease.
Drug-induced esophagitis
Treatment for drug-induced esophagitis is primarily avoiding the problem drug when possible and reducing the risk with better pill-taking habits. Your doctor may recommend:
- Taking an alternative drug that is less likely to cause drug-induced esophagitis
- Taking a liquid version of a medication if possible
- Drinking an entire glass of water with a pill, unless you've been told by your doctor to restrict your fluid intake because of another condition, such as kidney disease
- Sitting or standing for at least 30 minutes after taking a pill
Infectious esophagitis
Your doctor may prescribe a medication to treat a bacterial, viral, fungal or parasitic infection causing infectious esophagitis.
Treating common complications
A gastroenterologist may perform a procedure to expand (dilate) the esophagus. This treatment is generally used only when the narrowing is very severe or food has become lodged in the esophagus.
In esophageal dilation, your doctor uses one or more endoscopic devices — small narrow tubes inserted through the esophagus. Versions of these devices may be equipped with:
- A tapered tip that starts with a rounded point that gradually widens
- A balloon that can be expanded after it's inserted in the esophagus
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Esophagitis and Learn More about Diseases
Spermatocele
Ehlers-Danlos syndrome
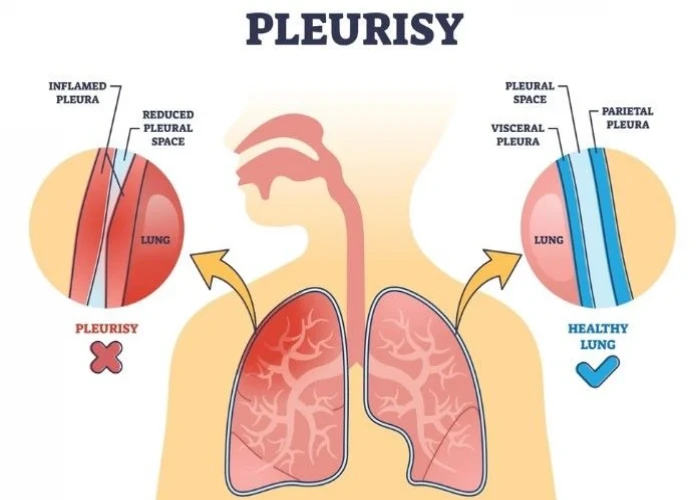
Pleurisy

Inflammatory bowel disease (IBD)

Hurthle cell cancer
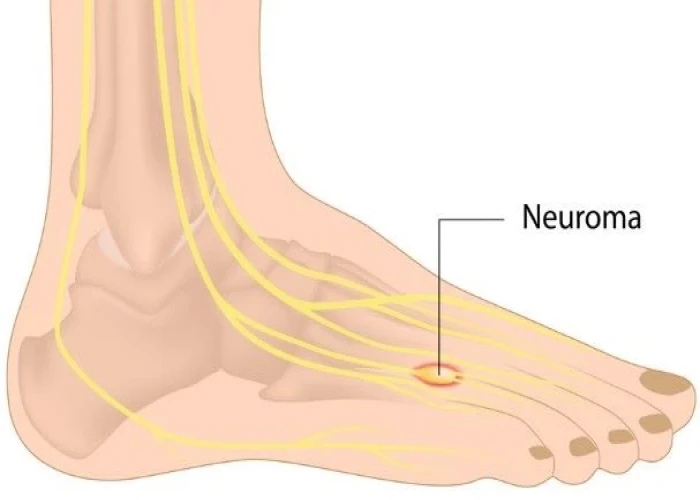
Morton's neuroma
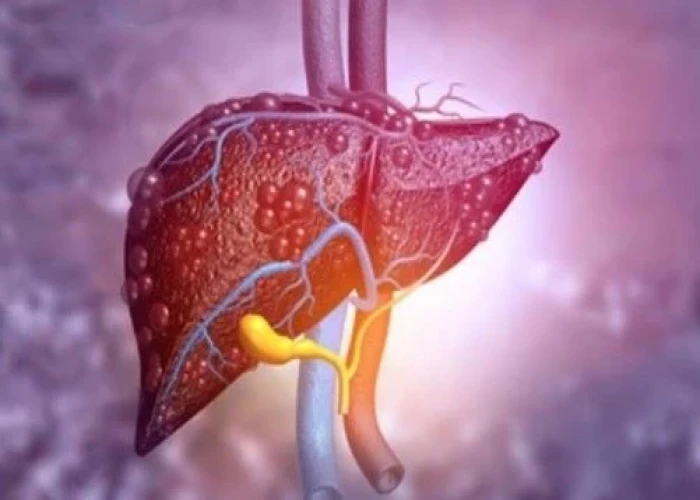
Primary sclerosing cholangitis

Encephalitis
esophagitis, খাদ্যনালী
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.