 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Vaginal atrophy

Vaginal atrophy, also known as atrophic vaginitis, is a condition that occurs when the vaginal tissues become thin, dry, and less elastic. It is a common condition that affects women, especially those who have gone through menopause, but it can also occur in women who are breastfeeding, using certain medications, or have undergone cancer treatment.
Symptoms of vaginal atrophy can include vaginal dryness, itching, burning, pain during intercourse, and urinary symptoms such as frequent urination or urinary incontinence. In some cases, vaginal bleeding or spotting may occur.
Diagnosis of vaginal atrophy typically involves a pelvic exam and a discussion of symptoms. In some cases, additional testing such as a biopsy or imaging may be required to rule out other conditions.
Treatment for vaginal atrophy depends on the severity of the condition and may include the use of vaginal moisturizers or lubricants to reduce dryness, hormone replacement therapy to replace declining estrogen levels, or low-dose vaginal estrogen therapy to restore vaginal tissue health. In some cases, non-hormonal treatments such as ospemifene may be used to alleviate symptoms.
Preventive measures for vaginal atrophy include regular sexual activity, staying hydrated, and avoiding irritants such as douching or using scented products in the vaginal area. It is important to discuss treatment options with a healthcare provider to determine the best course of action based on individual circumstances.
Research Papers
Disease Signs and Symptoms
- Vaginal dryness
- Decreased vaginal lubrication during sexual activity
- Bleeding with intercourse
- Frequent urination
- Unable to retain speed of urination
- Burning during urination
- Vaginal itching
- Itching
- Frequent menstruation
- Vaginal pain or burning
- Shortening and tightening of the vaginal canal
Disease Causes
Vaginal atrophy
Genitourinary syndrome of menopause is caused by a decrease in estrogen production. Less estrogen makes your vaginal tissues thinner, drier, less elastic and more fragile.
A drop in estrogen levels may occur:
- After menopause
- During the years leading up to menopause (perimenopause)
- After surgical removal of both ovaries (surgical menopause)
- During breast-feeding
- While taking medications that can affect estrogen levels, such as some birth control pills
- After pelvic radiation therapy for cancer
- After chemotherapy for cancer
- As a side effect of breast cancer hormonal treatment
GSM signs and symptoms may begin to bother you during the years leading up to menopause, or they may not become a problem until several years into menopause. Although the condition is common, not all menopausal women experience GSM. Regular sexual activity, with or without a partner, can help you maintain healthy vaginal tissues.
Disease Prevents
Vaginal atrophy
Regular sexual activity, either with or without a partner, may help prevent genitourinary syndrome of menopause. Sexual activity increases blood flow to your vagina, which helps keep vaginal tissues healthy.
Disease Treatments
To treat genitourinary syndrome of menopause, your doctor may first recommend over-the-counter treatment options, including:
- Vaginal moisturizers. Try a vaginal moisturizer (K-Y Liquibeads, Replens, Sliquid, others) to restore some moisture to your vaginal area. You may have to apply the moisturizer every few days. The effects of a moisturizer generally last a bit longer than those of a lubricant.
- Water-based lubricants. These lubricants (Astroglide, K-Y Jelly, Sliquid, others) are applied just before sexual activity and can reduce discomfort during intercourse. Choose products that don't contain glycerin or warming properties because women who are sensitive to these substances may experience irritation. Avoid petroleum jelly or other petroleum-based products for lubrication if you're also using condoms, because petroleum can break down latex condoms on contact.
If those options don't ease your symptoms, your doctor may recommend:
Topical estrogen
Vaginal estrogen has the advantage of being effective at lower doses and limiting your overall exposure to estrogen because less reaches your bloodstream. It may also provide better direct relief of symptoms than oral estrogen does.
Vaginal estrogen therapy comes in a number of forms. Because they all seem to work equally well, you and your doctor can decide which one is best for you.
- Vaginal estrogen cream (Estrace, Premarin). You insert this cream directly into your vagina with an applicator, usually at bedtime. Typically women use it daily for one to three weeks and then one to three times a week thereafter, but your doctor will let you know how much cream to use and how often to insert it.
- Vaginal estrogen suppositories (Imvexxy). These low-dose estrogen suppositories are inserted about 2 inches into the vaginal canal daily for weeks. Then, the suppositories only need to be inserted twice a week.
- Vaginal estrogen ring (Estring, Femring). You or your doctor inserts a soft, flexible ring into the upper part of the vagina. The ring releases a consistent dose of estrogen while in place and needs to be replaced about every three months. Many women like the convenience this offers. A different, higher dose ring is considered a systemic rather than topical treatment.
- Vaginal estrogen tablet (Vagifem). You use a disposable applicator to place a vaginal estrogen tablet in your vagina. Your doctor will let you know how often to insert the tablet. You might, for instance, use it daily for the first two weeks and then twice a week thereafter.
Ospemifene (Osphena)
Taken daily, this pill can help relieve painful sex symptoms in women with moderate to severe GSM. It is not approved in women who've had breast cancer or who have a high risk of developing breast cancer.
Prasterone (Intrarosa)
These vaginal inserts deliver the hormone DHEA directly to the vagina to help ease painful sex. DHEA is a hormone that helps the body produce other hormones, including estrogen. Prasterone is used nightly for moderate to severe vaginal atrophy.
Systemic estrogen therapy
If vaginal dryness is associated with other symptoms of menopause, such as moderate or severe hot flashes, your doctor may suggest estrogen pills, patches or gel, or a higher dose estrogen ring. Estrogen taken by mouth enters your entire system. Ask your doctor to explain the risks versus the benefits of oral estrogen, and whether or not you would also need to take another hormone called progestin along with estrogen.
Vaginal dilators
You may use vaginal dilators as a nonhormonal treatment option. Vaginal dilators may also be used in addition to estrogen therapy. These devices stimulate and stretch the vaginal muscles to reverse narrowing of the vagina.
If painful sex is a concern, vaginal dilators may relieve vaginal discomfort by stretching the vagina. They are available without a prescription, but if your symptoms are severe, your doctor may recommend pelvic floor physical therapy and vaginal dilators. Your health care provider or a pelvic physical therapist can teach you how to use vaginal dilators.
Topical lidocaine
Available as a prescription ointment or gel, topical lidocaine can be used to lessen discomfort associated with sexual activity. Apply it five to 10 minutes before you begin sexual activity.
If you've had breast cancer
If you have a history of breast cancer, tell your doctor and consider these options:
- Nonhormonal treatments. Try moisturizers and lubricants as a first choice.
- Vaginal dilators. Vaginal dilators are a nonhormonal option that can stimulate and stretch the vaginal muscles. This helps to reverse narrowing of the vagina.
- Vaginal estrogen. In consultation with your cancer specialist (oncologist), your doctor might recommend low-dose vaginal estrogen if nonhormonal treatments don't help your symptoms. However, there's some concern that vaginal estrogen might increase your risk of the cancer coming back, especially if your breast cancer was hormonally sensitive.
- Systemic estrogen therapy. Systemic estrogen treatment generally isn't recommended, especially if your breast cancer was hormonally sensitive.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Vaginal atrophy and Learn More about Diseases
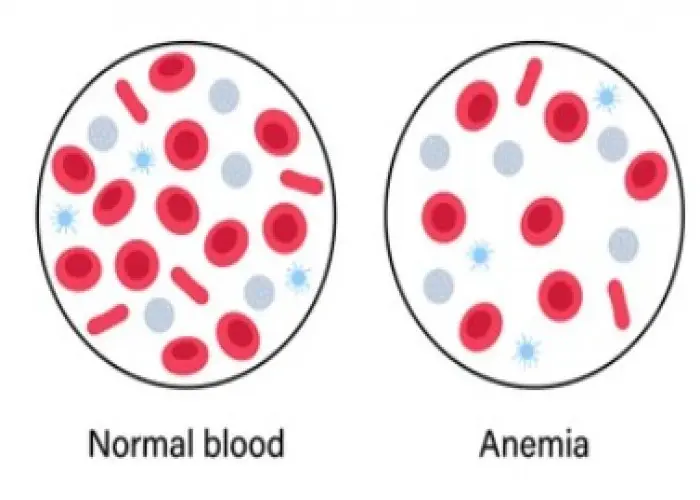
Anemia

Ataxia

Brucellosis
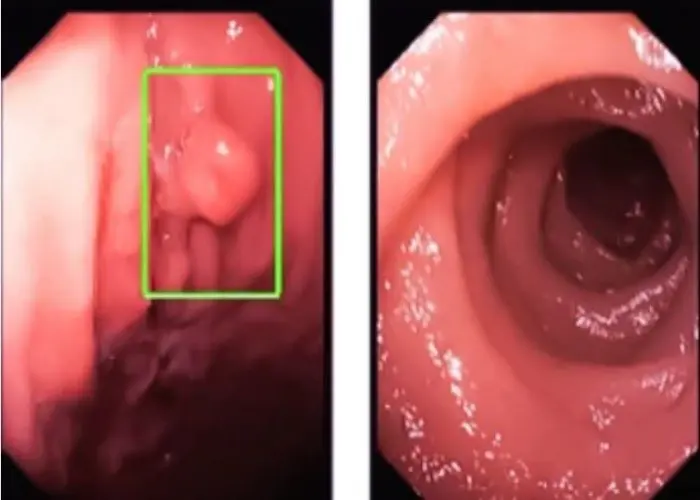
Colon polyps

Diabetic coma

Dry eyes

Myasthenia gravis
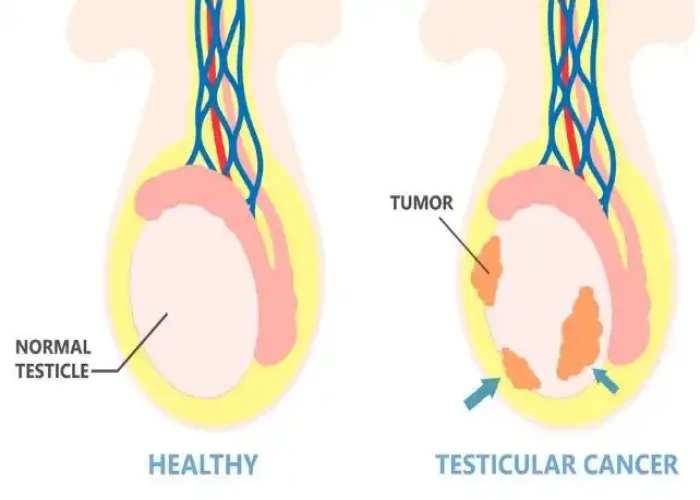
Undescended testicle
vaginal atrophy, ভ্যাজাইনাল অ্যাট্রোফি, যোনিপথের অ্যাট্রোফি
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
