Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
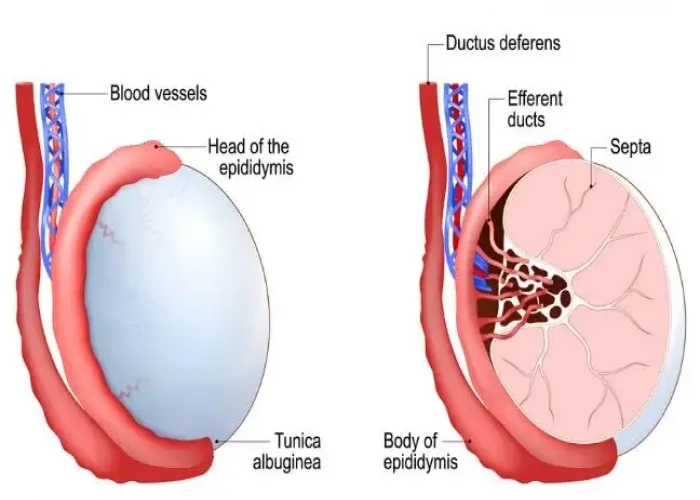
Spermatocele
A spermatocele, also known as a spermatic cyst, is a fluid-filled sac that forms in the epididymis, which is the tube that carries sperm from the testicles to the vas deferens. Spermatoceles are usually painless and often feel like a small, smooth lump located above or behind the testicle.
The exact cause of spermatoceles is not well understood, but they are thought to be related to blockages or obstructions in the epididymis. Spermatoceles are more common in men over the age of 40 and are typically not associated with any serious health risks.
Most spermatoceles do not require treatment unless they are causing significant discomfort or interfering with fertility. In some cases, a spermatocele may be surgically removed if it is large, causing discomfort, or affecting sperm production or quality. However, surgery is typically only recommended in cases where conservative treatments have not been effective.
If you notice a lump or swelling in your testicle or scrotum, it is important to seek medical attention for further evaluation and diagnosis. Your doctor can help determine if the lump is a spermatocele or another condition that may require treatment.
Research Papers
Disease Signs and Symptoms
- Testicle pain
- Heaviness in testicle with the spermatocele
- Fullness behind and above the testicle
Disease Causes
Spermatocele
The cause of spermatoceles is unknown. Spermatoceles might result from a blockage in one of the multiple tubes within the epididymis that transport and store sperm from the testicle.
Disease Prevents
Spermatocele
Although there's no way to prevent a spermatocele, it's important for you to conduct scrotal self-exams at least monthly to detect changes, such as masses, in your scrotum. Any new mass in your scrotum should be evaluated promptly.
Your doctor can instruct you in how to conduct a testicular self-examination, which can improve your chances of finding a mass.
How to examine your testicles
A good time to examine your testicles is during or after a warm bath or shower. The heat from the water relaxes your scrotum, making it easier for you to detect anything unusual. Then follow these steps:
- Stand in front of a mirror. Look for any swelling on the skin of the scrotum.
- Examine each testicle with both hands. Place the index and middle fingers under the testicle while placing your thumbs on the top.
- Gently roll the testicle between the thumbs and the fingers. Remember that the testicles are usually smooth, oval shaped and somewhat firm. It's normal for one testicle to be slightly larger than the other. Also, the cord leading upward from the top of the testicle (epididymis) is a normal part of the scrotum.
By regularly performing this exam, you'll become more familiar with your testicles and aware of any changes that might be of concern. If you find a lump, call your doctor as soon as possible.
Regular self-examination is an important health habit. But it can't substitute for a doctor's examination. Your doctor normally checks your testicles whenever you have a physical exam.
Disease Treatments
Although your spermatocele probably won't go away on its own, most spermatoceles don't need treatment. They generally don't cause pain or complications. If yours is painful, your doctor might recommend over-the-counter pain medications, such as acetaminophen (Tylenol, others) or ibuprofen (Advil, Motrin IB, others).
Surgical treatment
A procedure called a spermatocelectomy generally is performed on an outpatient basis, using a local or general anesthetic. The surgeon makes an incision in the scrotum and separates the spermatocele from the epididymis.
After surgery, you might need to wear a gauze-filled athletic supporter to apply pressure to and protect the site of the incision. Your doctor might also tell you to:
- Apply ice packs for two or three days to keep swelling down
- Take oral pain medications for a day or two
- Return for a follow-up exam between one and three weeks after surgery
Possible complications from surgical removal that might affect fertility include damage to the epididymis or to the tube that transports sperm (vas deferens). It's also possible that a spermatocele might come back, even after surgery.
Aspiration, with or without sclerotherapy
Other treatments include aspiration and sclerotherapy, though these are rarely used. During aspiration, a special needle is inserted into the spermatocele and fluid is removed (aspirated).
If the spermatocele recurs, your doctor might recommend aspirating the fluid again and then injecting an irritating chemical into the sac (sclerotherapy). The irritating agent causes the spermatocele sac to scar, which takes up the space the fluid occupied and lowers the risk of the spermatocele coming back.
Damage to the epididymis is a possible complication of sclerotherapy. It's also possible that your spermatocele might come back.
Protecting your fertility
Surgery can potentially cause damage to the epididymis or the vas deferens, and sclerotherapy might damage the epididymis, which can affect fertility. Because of this concern, these procedures might be delayed until you're done having children. If the spermatocele is causing so much discomfort that you don't want to wait, talk with your doctor about the risks and benefits of sperm banking.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Spermatocele and Learn More about Diseases
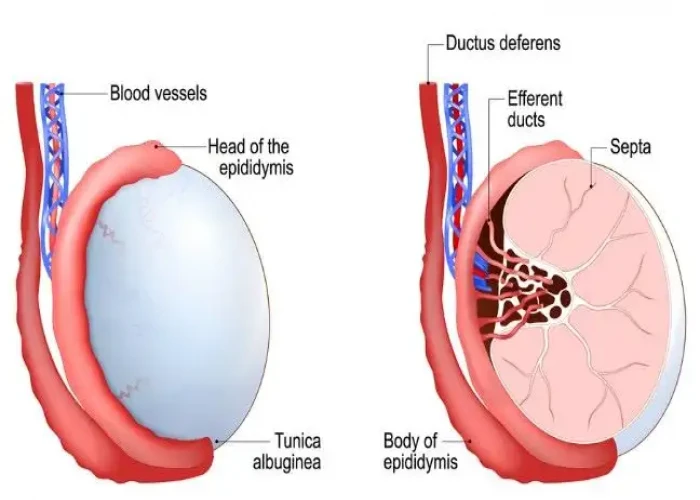
Ehrlichiosis and anaplasmosis

Tinea versicolor

Milk allergy
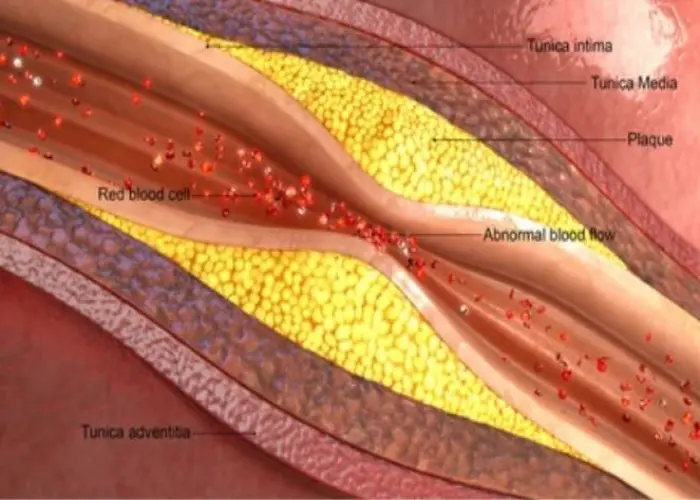
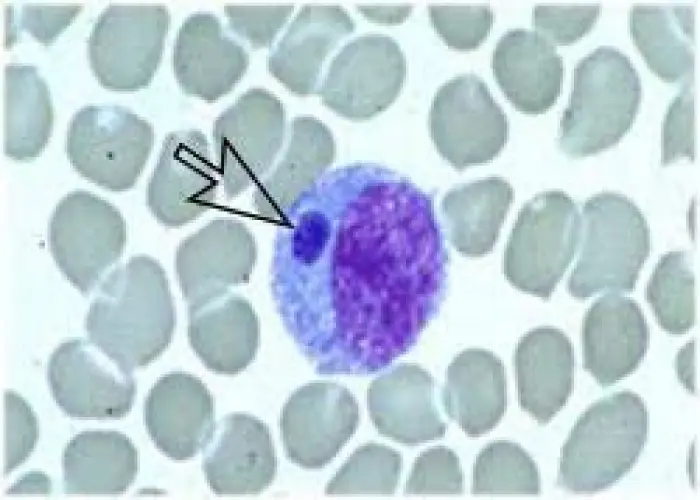
Arteriosclerosis / atherosclerosis
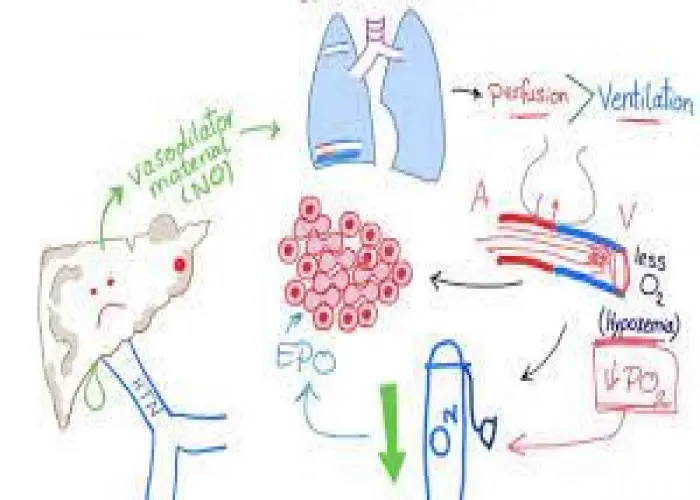
Hepatopulmonary syndrome

Perimenopause

Delayed sleep phase

Peyronie's disease
spermatocele, স্পার্মাটোসেল
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.