Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Primary biliary cholangitis
Primary biliary cholangitis (PBC) is a chronic liver disease that damages the bile ducts in the liver, leading to a buildup of bile in the liver and a decrease in the flow of bile to the intestines. This can lead to inflammation and scarring of the liver, which can eventually lead to cirrhosis and liver failure.
The cause of PBC is not fully understood, but it is believed to be an autoimmune disorder, in which the body's immune system attacks the bile ducts in the liver. Risk factors for PBC include being female, having a family history of the disease, and having other autoimmune disorders such as rheumatoid arthritis or thyroid disease.
Symptoms of PBC can include fatigue, itching, dry eyes and mouth, jaundice (yellowing of the skin and eyes), and abdominal pain. Many people with PBC are asymptomatic and the disease is often discovered during routine blood tests.
Treatment for PBC typically involves medications to slow the progression of the disease, such as ursodeoxycholic acid (UDCA). Other medications may be prescribed to manage symptoms such as itching. In severe cases, a liver transplant may be necessary.
Lifestyle changes such as avoiding alcohol, maintaining a healthy weight, and avoiding medications that can be toxic to the liver are also important in managing PBC.
Early diagnosis and treatment of PBC is important to prevent complications such as cirrhosis and liver failure. If you are experiencing symptoms or have risk factors for PBC, it is important to discuss your concerns with your healthcare provider.
Research Papers
Disease Signs and Symptoms
- Fatigue (Tiredness)
- High cholesterol
- Underactive thyroid (hypothyroidism)
- Weight loss
- Bone, muscle or joint (musculoskeletal) pain
- Buildup of fluid in the abdomen due to liver failure (ascites)
- Fatty deposits (xanthomas) on the skin around the eyes, eyelids or in the creases of the palms, soles, elbows or knees
- Darkening of the skin that's not related to sun exposure (hyperpigmentation)
- Weak and brittle bones (osteoporosis), which can lead to fractures
- Yellowing of skin and eyes (jaundice)
- Swollen feet and ankles (edema)
- Itching
- Dry eyes
- Dry mouth
- Upper abdomen pain
- Swollen spleen (splenomegaly)
- Bone pain
- Muscle pain
- Joint pain
- Diarrhea, which may include greasy stools (steatorrhea)
Disease Causes
Primary biliary cholangitis
It's not clear what causes primary biliary cholangitis. Many experts consider it an autoimmune disease in which the body turns against its own cells. Researchers believe this autoimmune response may be triggered by environmental and genetic factors.
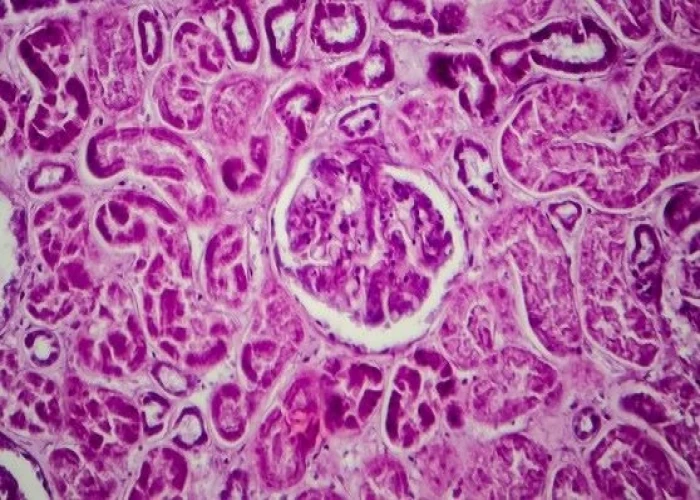
The liver inflammation seen in primary biliary cholangitis starts when certain types of white blood cells called T cells (T lymphocytes) start to collect in the liver. Normally, these immune cells detect and help defend against germs, such as bacteria and viruses. But in primary biliary cholangitis, they mistakenly destroy the healthy cells lining the small bile ducts in the liver.
Inflammation in the smallest ducts spreads and eventually damages other cells in the liver. As the cells die, they're replaced by scar tissue (fibrosis) that can lead to cirrhosis. Cirrhosis is scarring of liver tissue that makes it difficult for your liver to work properly.
Disease Prevents
Disease Treatments
Treating the disease
There's no cure for primary biliary cholangitis, but medications are available to help slow the progression of the disease and prevent complications. Options include:
- Ursodeoxycholic acid (UDCA). This medication, also known as ursodiol (Actigall, Urso), is commonly used first. It helps move bile through your liver. UDCA doesn't cure primary biliary cholangitis, but it seems to improve liver function and reduce liver scarring. It's less likely to help with itching and fatigue. Side effects may include weight gain, hair loss and diarrhea.
- Obeticholic acid (Ocaliva). In 2016, the U.S. Food and Drug Administration approved this medication for primary biliary cholangitis. Studies show that when given alone or combined with ursodiol for 12 months it can help improve liver function and slow liver fibrosis. However, its use is often limited because it can cause increased itching.
- Fibrates (Tricor). Researchers aren't exactly sure how this medicine works to help ease primary biliary cholangitis symptoms. But, when taken with UDCA, it has reduced liver inflammation and itching in some people. More studies are needed to determine long-term benefits.
- Budesonide. When combined with UDCA, the corticosteroid budesonide may be of potential benefit for primary biliary cholangitis. However, this drug is associated with steroid-related side effects for people with more advanced disease. More long-term trials are necessary before budesonide can be recommended for treating this condition.
- Liver transplant. When medications no longer control primary biliary cholangitis and the liver begins to fail, a liver transplant may help prolong life. A liver transplant replaces your diseased liver with a healthy one from a donor. Liver transplantation is associated with very good long-term outcomes for people with primary biliary cholangitis. However, sometimes the disease comes back several years later in the transplanted liver.
Treating the symptoms
Your doctor may recommend treatments to control the signs and symptoms of primary biliary cholangitis and make you more comfortable.
Treatment for fatigue
Primary biliary cholangitis causes fatigue. But your daily habits, proper diet and exercise, and other health conditions can affect how tired you feel. It is important to also be tested to exclude thyroid disease since it is more common in people with primary biliary cholangitis.
Treatment for itching
- Antihistamines such as diphenhydramine, hydroxyzine hydrochloride and loratadine are commonly used to reduce itching. They may help with sleep if itching keeps you awake.
- Cholestyramine is a powder that must be mixed with food or liquids.
- Rifampin is an antibiotic that may stop itching. Exactly how it does this is unknown. Researchers think it may block the brain's response to itch-inducing chemicals in the blood.
- Sertraline is a selective serotonin reuptake inhibitor (SSRI) that can help reduce the symptoms of itching.
- Opioid antagonists such as those containing naloxone and naltrexone may help itching related to liver disease. Like rifampin, these drugs seem to reduce the itching sensation by acting on your brain.
Treatment for dry eyes and mouth
Artificial tears and saliva substitutes, available over-the-counter or by prescription, can help ease dry eyes and mouth. Chewing gum or sucking on hard candy also can help you make more saliva and relieve dry mouth.
Treating the complications
Certain complications are commonly associated with primary biliary cholangitis. Your doctor may recommend:
- Vitamin and mineral supplements. If your body isn't absorbing vitamins or other nutrients, you may need to take vitamins A, D, E and K, as well as calcium, folic acid or iron supplements.
- Medication to lower cholesterol. If you have high cholesterol levels in your blood, your doctor may recommend taking a medication known as a statin.
- Drugs to treat bone loss. If you have weak or thinning bones (osteoporosis), you may be prescribed medication or supplements, such as calcium and vitamin D, to reduce bone loss and improve bone density. Exercise such as walking and using light weights most days of the week can help increase your bone density.
- Treatment for increased pressure in the portal vein (portal hypertension). Your doctor is likely to screen and monitor you for portal hypertension and enlarged veins if you have more advanced scarring (fibrosis or cirrhosis) from liver disease. Accumulating fluid in your abdomen (ascites) is a common side effect of portal hypertension. For mild fluid accumulation, your doctor may only recommend limiting salt in your diet. More-severe cases may require medications known as diuretics or a procedure to drain the fluid (paracentesis).
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Primary biliary cholangitis and Learn More about Diseases

Suspicious breast lumps

Lyme disease

Pectus excavatum
Lupus nephritis

Balance problems

Bronchiectasis
Gastrointestinal bleeding

Amnesia
primary biliary cholangitis, প্রাথমিক বিলিয়ারি কোলাঞ্জাইটিস
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.