Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
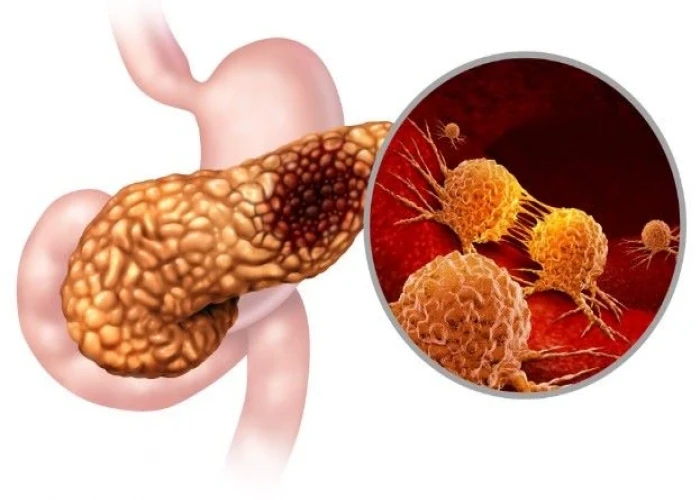
Pancreatic cancer

Pancreatic cancer is a type of cancer that starts in the pancreas, an organ located behind the stomach that plays an important role in digestion and the regulation of blood sugar. Pancreatic cancer can occur when cells in the pancreas grow and divide abnormally, forming a tumor.
Symptoms of pancreatic cancer may include:
- Abdominal pain or discomfort, especially in the upper abdomen or back
- Jaundice, which causes yellowing of the skin and eyes
- Unexplained weight loss
- Loss of appetite
- Fatigue
- Nausea and vomiting
- Changes in bowel movements
Risk factors for pancreatic cancer include smoking, obesity, a family history of pancreatic cancer or other related cancers, chronic pancreatitis, and certain genetic mutations.
Pancreatic cancer is typically diagnosed through imaging tests, such as CT scans or MRIs, as well as through a biopsy to examine a sample of tissue from the pancreas. Treatment options may include surgery to remove the tumor, chemotherapy, radiation therapy, or a combination of these approaches.
Pancreatic cancer can be difficult to treat, as it often does not cause noticeable symptoms until it has advanced. However, early detection and treatment can improve outcomes, so it's important to be aware of the symptoms and risk factors for pancreatic cancer and to seek medical attention promptly if any concerning symptoms arise.
Research Papers
Disease Signs and Symptoms
- Abdomen pain
- Loss of appetite
- Weight loss
- Yellowing of skin and eyes (jaundice)
- Dark urine color
- Itching
- Fatigue (Tiredness)
- New diagnosis of diabetes or existing diabetes that's becoming more difficult to control
- Persistent abdominal pain, which may radiate to back
Disease Causes
Pancreatic cancer
It's not clear what causes pancreatic cancer. Doctors have identified some factors that may increase the risk of this type of cancer, including smoking and having certain inherited gene mutations.
Understanding your pancreas
Your pancreas is about 6 inches (15 centimeters) long and looks something like a pear lying on its side. It releases (secretes) hormones, including insulin, to help your body process sugar in the foods you eat. And it produces digestive juices to help your body digest food and absorb nutrients.
How pancreatic cancer forms
Pancreatic cancer occurs when cells in your pancreas develop changes (mutations) in their DNA. A cell's DNA contains the instructions that tell a cell what to do. These mutations tell the cells to grow uncontrollably and to continue living after normal cells would die. These accumulating cells can form a tumor. When left untreated, the pancreatic cancer cells can spread to nearby organs and blood vessels and to distant parts of the body.
Most pancreatic cancer begins in the cells that line the ducts of the pancreas. This type of cancer is called pancreatic adenocarcinoma or pancreatic exocrine cancer. Less frequently, cancer can form in the hormone-producing cells or the neuroendocrine cells of the pancreas. These types of cancer are called pancreatic neuroendocrine tumors, islet cell tumors or pancreatic endocrine cancer.
Disease Prevents
Pancreatic cancer
You may reduce your risk of pancreatic cancer if you:
- Stop smoking. If you smoke, try to stop. Talk to your doctor about strategies to help you stop, including support groups, medications and nicotine replacement therapy. If you don't smoke, don't start.
- Maintain a healthy weight. If you are at a healthy weight, work to maintain it. If you need to lose weight, aim for a slow, steady weight loss — 1 to 2 pounds (0.5 to 1 kilogram) a week. Combine daily exercise with a diet rich in vegetables, fruit and whole grains with smaller portions to help you lose weight.
- Choose a healthy diet. A diet full of colorful fruits and vegetables and whole grains may help reduce your risk of cancer.
Consider meeting with a genetic counselor if you have a family history of pancreatic cancer. He or she can review your family health history with you and determine whether you might benefit from a genetic test to understand your risk of pancreatic cancer or other cancers.
Disease Treatments
Treatment for pancreatic cancer depends on the stage and location of the cancer as well as on your overall health and personal preferences. For most people, the first goal of pancreatic cancer treatment is to eliminate the cancer, when possible. When that isn't an option, the focus may be on improving your quality of life and limiting the cancer from growing or causing more harm.
Treatment may include surgery, radiation, chemotherapy or a combination of these. When pancreatic cancer is advanced and these treatments aren't likely to offer a benefit, your doctor will focus on symptom relief (palliative care) to keep you as comfortable as possible for as long as possible.
Surgery
Operations used in people with pancreatic cancer include:
- Surgery for tumors in the pancreatic head. If your cancer is located in the head of the pancreas, you may consider an operation called a Whipple procedure (pancreaticoduodenectomy).
- The Whipple procedure is a technically difficult operation to remove the head of the pancreas, the first part of the small intestine (duodenum), the gallbladder, part of the bile duct and nearby lymph nodes. In some situations, part of the stomach and colon may be removed as well. Your surgeon reconnects the remaining parts of your pancreas, stomach and intestines to allow you to digest food.
- Surgery for tumors in the pancreatic body and tail. Surgery to remove the left side (body and tail) of the pancreas is called distal pancreatectomy. Your surgeon may also need to remove your spleen.
- Surgery to remove the entire pancreas. In some people, the entire pancreas may need to be removed. This is called total pancreatectomy. You can live relatively normally without a pancreas but do need lifelong insulin and enzyme replacement.
- Surgery for tumors affecting nearby blood vessels. Many people with advanced pancreatic cancer aren't considered eligible for the Whipple procedure or other pancreatic surgeries if their tumors involve nearby blood vessels. At highly specialized and experienced medical centers, surgeons may offer pancreatic surgery operations that include removing and reconstructing affected blood vessels.
Each of these surgeries carries the risk of bleeding and infection. After surgery some people experience nausea and vomiting if the stomach has difficulty emptying (delayed gastric emptying). Expect a long recovery after any of these procedures. You'll spend several days in the hospital and then recover for several weeks at home.
Extensive research shows pancreatic cancer surgery tends to cause fewer complications when done by highly experienced surgeons at centers that do many of these operations. Don't hesitate to ask about your surgeon's and hospital's experience with pancreatic cancer surgery. If you have any doubts, get a second opinion.
Chemotherapy
Chemotherapy uses drugs to help kill cancer cells. These drugs can be injected into a vein or taken orally. You may receive one chemotherapy drug or a combination of them.
Chemotherapy can also be combined with radiation therapy (chemoradiation). Chemoradiation is typically used to treat cancer that hasn't spread beyond the pancreas to other organs. At specialized medical centers, this combination may be used before surgery to help shrink the tumor. Sometimes it is used after surgery to reduce the risk that pancreatic cancer may recur.
In people with advanced pancreatic cancer and cancer that has spread to other parts of the body, chemotherapy may be used to control cancer growth, relieve symptoms and prolong survival.
Radiation therapy
Radiation therapy uses high-energy beams, such as those made from X-rays and protons, to destroy cancer cells. You may receive radiation treatments before or after cancer surgery, often in combination with chemotherapy. Or your doctor may recommend a combination of radiation and chemotherapy treatments when your cancer can't be treated surgically.
Radiation therapy usually comes from a machine that moves around you, directing radiation to specific points on your body (external beam radiation). In specialized medical centers, radiation therapy may be delivered during surgery (intraoperative radiation).
Traditional radiation therapy uses X-rays to treat cancer, but a newer form of radiation using protons is available at some medical centers. In certain situations, proton therapy can be used to treat pancreatic cancer and it may offer fewer side effects compared with standard radiation therapy.
Clinical trials
Clinical trials are studies to test new treatments, such as systemic therapy, and new approaches to surgery or radiation therapy. If the treatment being studied proves to be safer and more effective than current treatments, it can become the new standard of care.
Clinical trials for pancreatic cancer might give you a chance to try new targeted therapy, chemotherapy drugs, immunotherapy treatments or vaccines.
Clinical trials can't guarantee a cure, and they might have serious or unexpected side effects. On the other hand, cancer clinical trials are closely monitored to ensure they're conducted as safely as possible. And they offer access to treatments that wouldn't otherwise be available to you.
Talk to your doctor about what clinical trials might be appropriate for you.
Supportive (palliative) care
Palliative care is specialized medical care that focuses on providing relief from pain and other symptoms of a serious illness. Palliative care is not the same as hospice care or end-of-life care. Palliative care is provided by teams of doctors, nurses, social workers and other specially trained professionals. These teams aim to improve the quality of life for people with cancer and their families.
Palliative care specialists work with you, your family and your other doctors to provide an extra layer of support that complements your ongoing medical care. It's often used while undergoing aggressive treatments, such as surgery, chemotherapy and radiation therapy.
When palliative care is used along with other appropriate treatments — even soon after the diagnosis — people with cancer may feel better and live longer.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Pancreatic cancer and Learn More about Diseases
Depersonalization-derealization disorder

Parvovirus infection

Nicotine dependence

Stress incontinence

Non-Hodgkin's lymphoma

Hyperthyroidism (Overactive Thyroid)

Ear infection (middle ear)

Periodontitis (Pyrrhoea)
pancreatic cancer, অগ্ন্যাশয়ের ক্যান্সার
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.