 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Intracranial hematoma
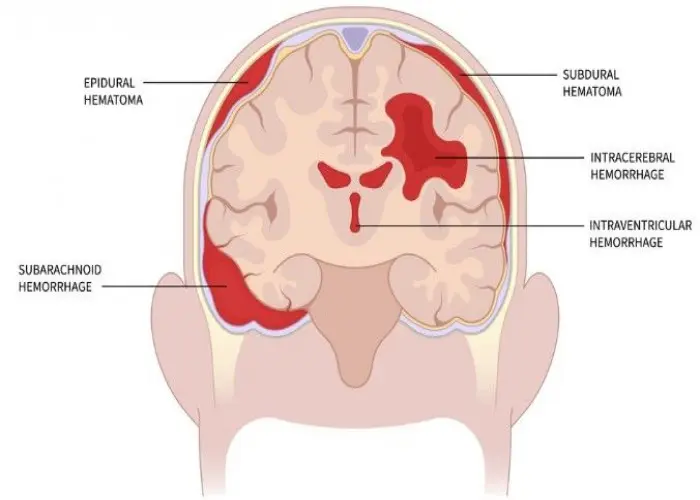
Intracranial hematoma is a type of traumatic brain injury that occurs when blood collects and forms a clot within the skull. The clot can cause pressure to build up in the brain, which can lead to brain damage or death if left untreated.
There are different types of intracranial hematoma, depending on the location of the clot within the skull. These include:
- Epidural hematoma: a clot that forms between the skull and the outermost layer of the brain (the dura mater)
- Subdural hematoma: a clot that forms between the dura mater and the middle layer of the brain (the arachnoid mater)
- Subarachnoid hematoma: a clot that forms in the cerebrospinal fluid-filled space between the arachnoid mater and the innermost layer of the brain (the pia mater)
- Intracerebral hematoma: a clot that forms within the brain tissue itself
Intracranial hematoma can occur as a result of a head injury or trauma, such as a fall, car accident, or assault. Symptoms of intracranial hematoma may include headache, confusion, dizziness, nausea and vomiting, seizures, and loss of consciousness.
Diagnosis of intracranial hematoma may involve a comprehensive medical evaluation, including a physical examination, imaging tests such as CT scan or MRI, and possibly a cerebral angiogram to evaluate blood flow in the brain. Treatment for intracranial hematoma may depend on the location and severity of the clot, and may include medications to control bleeding or reduce pressure in the brain, surgery to remove the clot or relieve pressure, or supportive care to manage symptoms and prevent complications.
Preventing intracranial hematoma may involve taking precautions to avoid head injuries or trauma, such as wearing helmets while participating in sports or riding a bike, using seat belts while driving, and practicing safe behaviors to avoid falls or accidents. It is important for individuals who have experienced a head injury to seek prompt medical attention if they develop symptoms of intracranial hematoma, as this condition can be life-threatening if left untreated.
Research Papers
Disease Signs and Symptoms
- Headaches
- Loss of movement (paralysis) on the opposite side of the body from the head injury
- Drowsiness and progressive loss of consciousness
- Blurred vision of eye
- Seizures
- Paralysis
- Slurred speech
- Unequal pupil size
- Confusion (Hallucinations)
- Dizziness (vertigo)
- Nausea or vomiting
- Stool mixed with blood and mucus sometimes referred to as current jelly stool because of its appearance
Disease Causes
Intracranial hematoma
A head injury is the most common cause of bleeding within the skull. A head injury may result from motor vehicle or bicycle accidents, falls, assaults, and sports injuries.
If you're an older adult, even mild head trauma can cause a hematoma. This is especially true if you're taking a blood-thinning medication or an anti-platelet drug, such as aspirin.
You can have a serious injury even if there's no open wound, bruise or other obvious damage.
There are three categories of hematoma — subdural hematoma, epidural hematoma and intracerebral (intraparenchymal) hematoma.
Subdural hematoma
This occurs when blood vessels — usually veins — rupture between your brain and the outermost of three membrane layers that cover your brain (dura mater). The leaking blood forms a hematoma that presses on the brain tissue. An enlarging hematoma can cause gradual loss of consciousness and possibly death.
The three types of subdural hematomas are:
- Acute. This most dangerous type is generally caused by a severe head injury, and signs and symptoms usually appear immediately.
- Subacute. Signs and symptoms take time to develop, sometimes days or weeks after your injury.
- Chronic. The result of less severe head injuries, this type of hematoma can cause slow bleeding, and symptoms can take weeks and even months to appear. You might not recall injuring your head. For example, bumping your head while getting into the car can cause bleeding, especially if you're on blood-thinning medication.
All three types require medical attention as soon as signs and symptoms appear so that permanent brain damage can be prevented.
The risk of subdural hematoma increases as you age. The risk is also greater for people who:
- Take aspirin or other blood-thinning medication daily
- Misuse alcohol
Epidural hematoma
Also called an extradural hematoma, this type occurs when a blood vessel — usually an artery — ruptures between the outer surface of the dura mater and the skull. Blood then leaks between the dura mater and the skull to form a mass that presses on brain tissue. The most common cause of an epidural hematoma is trauma.
Some people with this type of injury remain conscious, but most become drowsy or go into a coma from the moment of trauma. An epidural hematoma that affects an artery in your brain can be deadly without prompt treatment.
Intracerebral (intraparenchymal) hematoma
This type of hematoma, also known as intraparenchymal hematoma, occurs when blood pools in the tissues of the brain. There are many causes, including trauma, rupture of a bulging blood vessel (aneurysm), poorly connected arteries and veins from birth, high blood pressure, and tumors. Diseases can cause spontaneous leakage of blood into the brain. A head trauma can result in multiple severe intracerebral hematomas.
Disease Prevents
Intracranial hematoma
To prevent or minimize head injury:
- Wear a helmet and make sure your kids wear helmets. Wear an appropriate and properly fitted helmet when playing contact sports, bicycling, motorcycling, skiing, horseback riding, skating, skateboarding, snowboarding or doing any activity that could result in head injury.
- Buckle your seat belt and make sure your kids are buckled in. Do so every time you drive or ride in a motor vehicle.
- Protect young children. Always use properly fitted car seats, pad countertops and edges of tables, block stairways, tether heavy furniture or appliances to the wall to prevent tipping, and keep children from climbing on unsafe or unsteady objects.
Disease Treatments
Hematomas that are small and produce no signs or symptoms don't need to be removed. However, signs and symptoms can appear or worsen days or weeks after the injury. As a result, you might have to be watched for neurological changes, have your intracranial pressure monitored and undergo repeated head CT scans.
If you take blood-thinning medication, such as warfarin (Coumadin, Jantoven), you may need therapy to reverse the effects of the medication. This will reduce the risk of further bleeding. Options for reversing blood thinners include administering vitamin K and fresh frozen plasma.
Surgery
Hematoma treatment often involves surgery. The type of surgery depends on the type of hematoma you have. Options include:
- Surgical drainage. If the blood is localized and has transitioned from a solid clot to a liquid consistency, your doctor might create a small hole in your skull and use suction to remove the liquid.
- Craniotomy. Large hematomas might require that a section of your skull be opened (craniotomy) to remove the blood.
Recovery
Recovery after an intracranial hematoma can take a long time, and you might not recover completely. The greatest period of recovery is up to three months after the injury, usually with lesser improvement after that. If you continue to have neurological problems after treatment, you might need occupational and physical therapy.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Intracranial hematoma and Learn More about Diseases
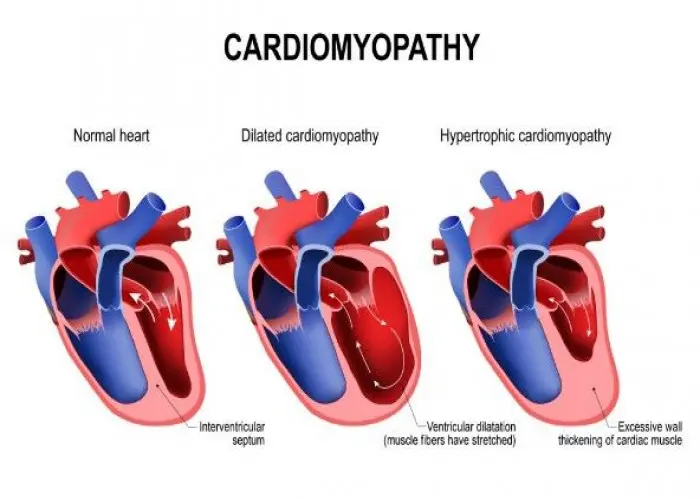
Dilated cardiomyopathy

Phenylketonuria (PKU)

Blood in urine (Hematuria)

Sprained ankle
Myelofibrosis

Impetigo

Leprosy
Angiosarcoma
intracranial hematoma, ইন্ট্রাক্রানিয়াল হেমাটোমা
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
