 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Group B strep disease

Group B strep disease, also known as GBS disease, is an infection caused by the bacterium Streptococcus agalactia. This bacterium is commonly found in the gastrointestinal and vaginal tracts of healthy adults.
GBS can cause a variety of infections in both adults and infants. In adults, GBS can cause urinary tract infections, pneumonia, and blood infections. In infants, GBS can cause sepsis (a serious blood infection), pneumonia, and meningitis.
Pregnant women can also carry GBS and may pass the bacterium to their newborn during delivery. Newborns who are infected with GBS can experience serious complications, including sepsis, meningitis, and pneumonia.
Testing for GBS is typically done during the third trimester of pregnancy. If a woman tests positive for GBS, she will be given antibiotics during labor to prevent transmission of the bacterium to her newborn.
Treatment for GBS disease in both adults and infants typically involves the use of antibiotics. However, it is important to note that GBS strains can differ in their resistance to certain antibiotics, so proper testing and identification of the specific strain are important for effective treatment.
Prevention of GBS disease in newborns can be achieved through proper prenatal care and screening, as well as timely administration of antibiotics during labor for women who test positive for GBS. It is important for individuals to consult with a healthcare professional to determine the best course of prevention and treatment for GBS disease.
Research Papers
Disease Signs and Symptoms
- Fever
- Fever and chills
- Yellowing of skin and eyes (jaundice)
- Skin rash
- Seizures
- Irritability
- Difficulty breathing (dyspnea)
- Weak muscle tone (hypotonia)
- Low body temperature
- Cough
Disease Causes
Group B strep disease
Many healthy people carry group B strep bacteria in their bodies. You might carry the bacteria in your body for a short time — it can come and go — or you might always have it. Group B strep bacteria aren't sexually transmitted, and they're not spread through food or water. How the bacteria are spread to anyone other than newborns isn't known.
Group B strep can spread to a baby during a vaginal delivery if the baby is exposed to — or swallows — fluids containing group B strep.
Disease Prevents
Group B strep disease
If you're pregnant, the American College of Obstetricians and Gynecologists recommends a group B strep screening during weeks 36 to 37 of pregnancy. Your doctor will take swab samples from your vagina and rectum and send them to a lab for testing.
A positive test indicates that you carry group B strep. It doesn't mean that you're ill or that your baby will be affected, but that you're at increased risk of passing the bacteria to your baby.
To prevent group B bacteria from spreading to your baby during labor or delivery, your doctor can give you an IV antibiotic — usually penicillin or a related drug — when labor begins.
If you're allergic to penicillin or related drugs, you might receive clindamycin or vancomycin as an alternative. Because the effectiveness of these alternatives is not well understood, your baby will be monitored for up to 48 hours.
Taking oral antibiotics ahead of time won't help because the bacteria can return before labor begins.
Antibiotic treatment during labor is also recommended if you:
- Have a urinary tract infection
- Delivered a previous baby with group B strep disease
- Develop a fever during labor
- Haven't delivered your baby within 18 hours of your water breaking
- Go into labor before 37 weeks and haven't been tested for group B strep
Vaccine in development
Although it's not available yet, researchers are working on a group B strep vaccine that could help prevent group B strep infections in the future.
Disease Treatments
Infants
If your baby tests positive for group B strep, he or she will be given intravenous (IV) antibiotics. Depending on your baby's condition, he or she might need IV fluids, oxygen or other medications.
Adults
Antibiotics are effective treatment for group B strep infection in adults. The choice of antibiotic depends on the location and extent of the infection and your specific circumstances.
If you're pregnant and you develop complications due to group B strep, you'll be given oral antibiotics, usually penicillin, amoxicillin (Amoxil, Larotid) or cephalexin (Keflex). All are considered safe to take during pregnancy.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Group B strep disease and Learn More about Diseases

Hyperhidrosis

Broken hand

Anal cancer

Urinary incontinence
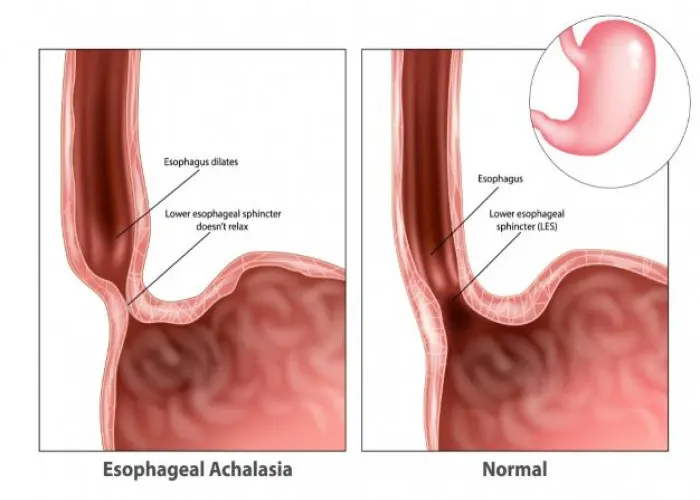
Achalasia
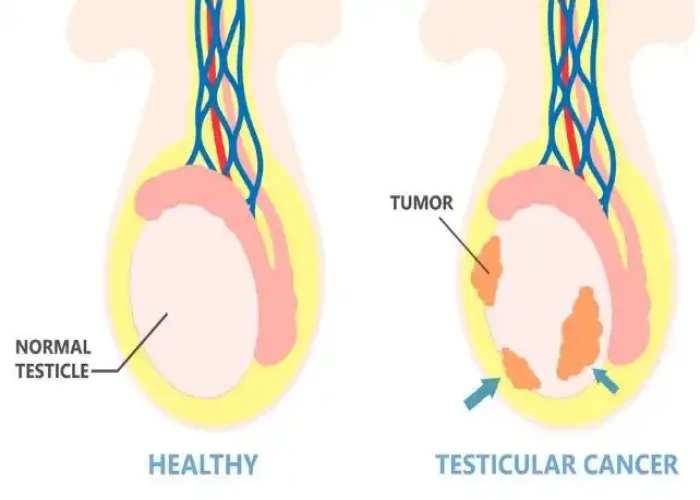
Undescended testicle

Uterine fibroids

Sacral dimple
group b strep disease, গ্রুপ বি স্ট্রেপ ডিজিজ
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
