 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Gestational diabetes

Gestational diabetes is a type of diabetes that develops during pregnancy. It is caused by hormonal changes that make it more difficult for the body to produce and use insulin effectively.
Gestational diabetes usually develops in the second or third trimester of pregnancy and affects about 6-9% of pregnancies in the United States. Women who have a higher risk of developing gestational diabetes include those who are overweight, have a family history of diabetes, have had gestational diabetes in a previous pregnancy, or are older than 25 years of age.
Symptoms of gestational diabetes may include increased thirst, frequent urination, blurred vision, and fatigue. However, many women with gestational diabetes may not have any symptoms at all.
Gestational diabetes can be diagnosed with a glucose screening test between 24-28 weeks of pregnancy. If the screening test indicates high blood sugar levels, a follow-up glucose tolerance test may be needed to confirm the diagnosis.
Treatment for gestational diabetes usually involves making lifestyle changes, such as eating a healthy diet, getting regular exercise, and monitoring blood sugar levels. In some cases, medication or insulin may be needed to help manage blood sugar levels.
If left untreated, gestational diabetes can lead to complications such as preterm labor, preeclampsia, or larger-than-average babies. However, with proper treatment and monitoring, most women with gestational diabetes have healthy pregnancies and babies. It is important to seek medical attention if you suspect you may have gestational diabetes or if you have any concerns about your pregnancy.
Research Papers
Disease Signs and Symptoms
- Diabetes
- High blood sugar
Disease Causes
Gestational diabetes
Researchers don't yet know why some women get gestational diabetes and others don't. Excess weight before pregnancy often plays a role.
Normally, various hormones work to keep your blood sugar levels in check. But during pregnancy, hormone levels change, making it harder for your body to process blood sugar efficiently. This makes your blood sugar rise.
Disease Prevents
Gestational diabetes
There are no guarantees when it comes to preventing gestational diabetes — but the more healthy habits you can adopt before pregnancy, the better. If you've had gestational diabetes, these healthy choices may also reduce your risk of having it again in future pregnancies or developing type 2 diabetes in the future.
- Eat healthy foods. Choose foods high in fiber and low in fat and calories. Focus on fruits, vegetables and whole grains. Strive for variety to help you achieve your goals without compromising taste or nutrition. Watch portion sizes.
- Keep active. Exercising before and during pregnancy can help protect you from developing gestational diabetes. Aim for 30 minutes of moderate activity on most days of the week. Take a brisk daily walk. Ride your bike. Swim laps. Short bursts of activity — such as parking further away from the store when you run errands or taking a short walk break — all add up too.
- Start pregnancy at a healthy weight. If you're planning to get pregnant, losing extra weight beforehand may help you have a healthier pregnancy. Focus on making lasting changes to your eating habits that can help you through pregnancy, such as eating more vegetables and fruits.
- Don't gain more weight than recommended. Gaining some weight during pregnancy is normal and healthy. But gaining too much weight too quickly can up your risk of gestational diabetes. Ask your doctor what a reasonable amount of weight gain is for you.
Disease Treatments
Treatment for gestational diabetes includes:
- Lifestyle changes
- Blood sugar monitoring
- Medication, if necessary
Managing your blood sugar levels helps keep you and your baby healthy. Close management can also help you avoid complications during pregnancy and delivery.
Lifestyle changes
Your lifestyle — how you eat and move — is an important part of keeping your blood sugar levels in a healthy range. Doctors don't advise losing weight during pregnancy — your body is working hard to support your growing baby. But your doctor can help you set weight gain goals based on your weight before pregnancy.
Healthy diet
A healthy diet focuses on fruits, vegetables, whole grains and lean protein — foods that are high in nutrition and fiber and low in fat and calories — and limits highly refined carbohydrates, including sweets. A registered dietitian or a diabetes educator can help you create a meal plan based on your current weight, pregnancy weight gain goals, blood sugar level, exercise habits, food preferences and budget.
Stay active
Regular physical activity plays a key role in every woman's wellness plan before, during and after pregnancy. Exercise lowers your blood sugar, and as an added bonus, regular exercise can help relieve some common discomforts of pregnancy, including back pain, muscle cramps, swelling, constipation and trouble sleeping.
With your doctor's OK, aim for 30 minutes of moderate exercise on most days of the week. If you haven't been active for a while, start slowly and build up gradually. Walking, cycling and swimming are good choices during pregnancy. Everyday activities such as housework and gardening also count.
Monitor your blood sugar
While you're pregnant, your health care team may ask you to check your blood sugar four or more times a day — first thing in the morning and after meals — to make sure your level stays within a healthy range.
Medication
If diet and exercise aren't enough, you may need insulin injections to lower your blood sugar. Between 10% and 20% of women with gestational diabetes need insulin to reach their blood sugar goals. Some doctors prescribe an oral medication to control blood sugar, while others believe more research is needed to confirm that oral drugs are as safe and as effective as injectable insulin to control gestational diabetes.
Close monitoring of your baby
An important part of your treatment plan is close observation of your baby. Your doctor may check your baby's growth and development with repeated ultrasounds or other tests. If you don't go into labor by your due date — or sometimes earlier — your doctor may induce labor. Delivering after your due date may increase the risk of complications for you and your baby.
Follow-up after delivery
Your doctor will check your blood sugar after delivery and again in six to 12 weeks to make sure that your level has returned to normal. If your tests are normal — and most are — you'll need to have your diabetes risk assessed at least every three years.
If future tests indicate type 2 diabetes or prediabetes, talk with your doctor about increasing your prevention efforts or starting a diabetes management plan.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Gestational diabetes and Learn More about Diseases
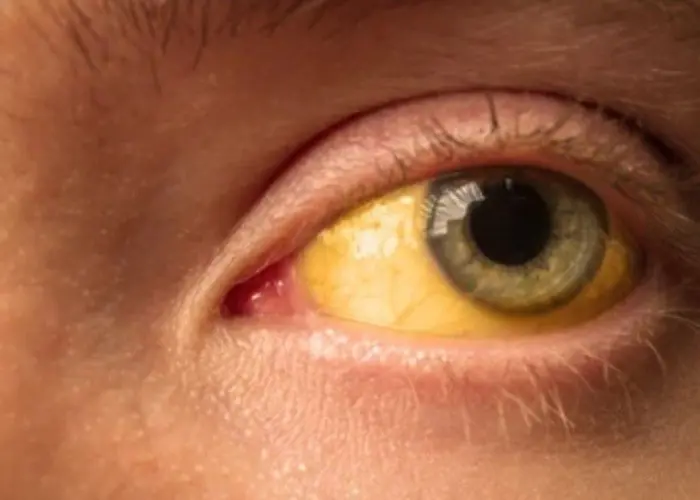
Cirrhosis
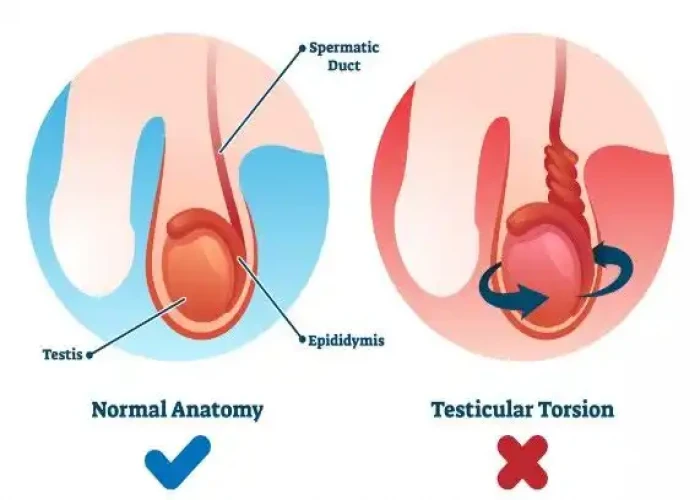
Testicular torsion

Posterior vaginal prolapse (Rectocele)

Common cold
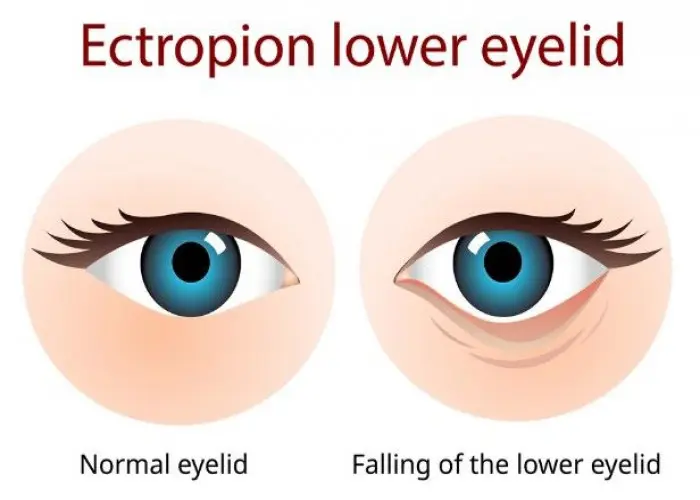
Ectropion

Heart arrhythmia

Costochondritis

Factor V Leiden
gestational diabetes, গর্ভাবস্থার ডায়াবেটিস
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
