Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
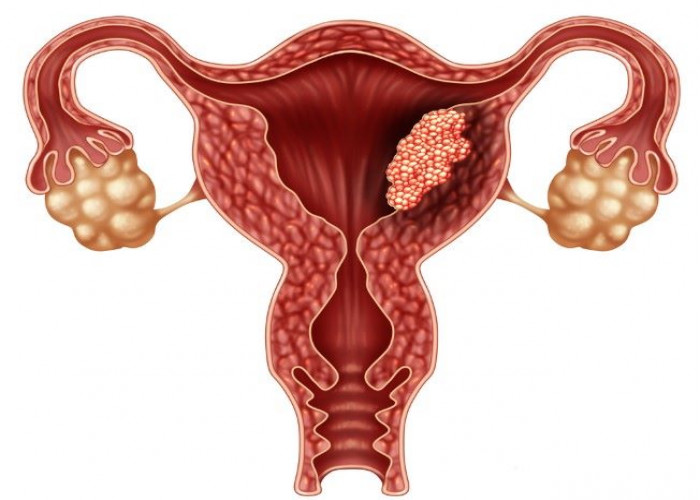
Endometrial cancer
Endometrial cancer is a type of cancer that starts in the lining of the uterus, which is called the endometrium. It is the most common type of uterine cancer, and it typically affects women after menopause, although it can occur in younger women as well.
The exact cause of endometrial cancer is not known, but it is thought to be related to a combination of genetic and hormonal factors. Women who have an early onset of menstruation, late onset of menopause, or who have never been pregnant may be at higher risk for endometrial cancer, as well as women who have a family history of the disease or who have a history of certain medical conditions, such as polycystic ovary syndrome.
Symptoms of endometrial cancer can include abnormal vaginal bleeding or discharge, pelvic pain, and pain during sex. However, in some cases, there may be no symptoms at all.
Diagnosis of endometrial cancer typically involves a combination of imaging tests, such as ultrasound or MRI, and a biopsy of the endometrial tissue to confirm the presence of cancer. Treatment usually involves surgery to remove the uterus and surrounding tissues, as well as radiation therapy and/or chemotherapy to kill any remaining cancer cells.
Prognosis for endometrial cancer is generally good, especially if the cancer is caught early and has not spread beyond the uterus. However, the outcome can vary depending on the stage and aggressiveness of the cancer, as well as the age and overall health of the patient. Regular screening, including pelvic exams and Pap tests, can help detect endometrial cancer early and improve the chances of successful treatment.
Research Papers
Disease Signs and Symptoms
- Vaginal bleeding
- Pelvic pain
- Vaginal bleeding between periods, such as after vaginal intercourse
Disease Causes
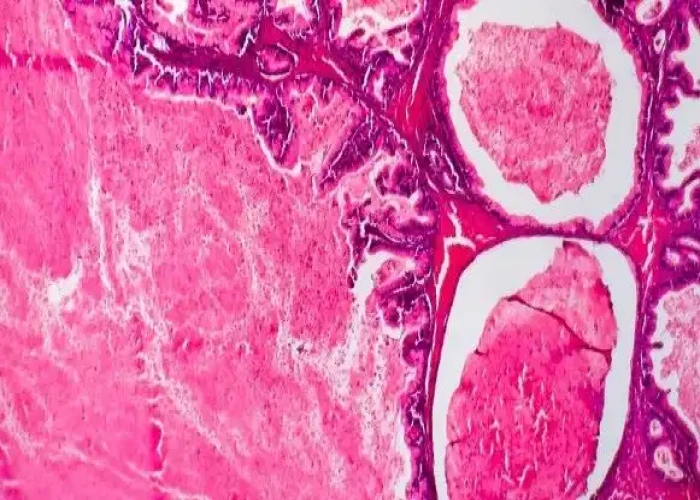
Endometrial cancer
Doctors don't know what causes endometrial cancer. What's known is that something occurs to create changes (mutations) in the DNA of cells in the endometrium — the lining of the uterus.
The mutation turns normal, healthy cells into abnormal cells. Healthy cells grow and multiply at a set rate, eventually dying at a set time. Abnormal cells grow and multiply out of control, and they don't die at a set time. The accumulating abnormal cells form a mass (tumor). Cancer cells invade nearby tissues and can separate from an initial tumor to spread elsewhere in the body (metastasize).
Disease Prevents
Endometrial cancer
To reduce your risk of endometrial cancer, you may wish to:
- Talk to your doctor about the risks of hormone therapy after menopause. If you're considering hormone replacement therapy to help control menopause symptoms, talk to your doctor about the risks and benefits. Unless you've undergone a hysterectomy, replacing estrogen alone after menopause may increase your risk of endometrial cancer. Taking a combination of estrogen and progestin can reduce this risk. Hormone therapy carries other risks, so weigh the benefits and risks with your doctor.
- Consider taking birth control pills. Using oral contraceptives for at least one year may reduce endometrial cancer risk. The risk reduction is thought to last for several years after you stop taking oral contraceptives. Oral contraceptives have side effects, though, so discuss the benefits and risks with your doctor.
- Maintain a healthy weight. Obesity increases the risk of endometrial cancer, so work to achieve and maintain a healthy weight. If you need to lose weight, increase your physical activity and reduce the number of calories you eat each day.
Disease Treatments
Treatment for endometrial cancer is usually with surgery to remove the uterus, fallopian tubes and ovaries. Another option is radiation therapy with powerful energy. Drug treatments for endometrial cancer include chemotherapy with powerful drugs and hormone therapy to block hormones that cancer cells rely on. Other options might be targeted therapy with drugs that attack specific weaknesses in the cancer cells and immunotherapy to help your immune system fight cancer.
Surgery
Treatment for endometrial cancer usually involves an operation to remove the uterus (hysterectomy), as well as to remove the fallopian tubes and ovaries (salpingo-oophorectomy). A hysterectomy makes it impossible for you to become pregnant in the future. Also, once your ovaries are removed, you'll experience menopause, if you haven't already.
During surgery, your surgeon will also inspect the areas around your uterus to look for signs that cancer has spread. Your surgeon may also remove lymph nodes for testing. This helps determine your cancer's stage.
Radiation therapy
Radiation therapy uses powerful energy beams, such as X-rays and protons, to kill cancer cells. In some instances, your doctor may recommend radiation to reduce your risk of a cancer recurrence after surgery. In certain situations, radiation therapy may also be recommended before surgery, to shrink a tumor and make it easier to remove.
If you aren't healthy enough to undergo surgery, you may opt for radiation therapy only.
Radiation therapy can involve:
- Radiation from a machine outside your body. During external beam radiation, you lie on a table while a machine directs radiation to specific points on your body.
- Radiation placed inside your body. Internal radiation (brachytherapy) involves placing a radiation-filled device, such as small seeds, wires or a cylinder, inside your vagina for a short period of time.
Chemotherapy
Chemotherapy uses chemicals to kill cancer cells. You may receive one chemotherapy drug, or two or more drugs can be used in combination. You may receive chemotherapy drugs by pill (orally) or through your veins (intravenously). These drugs enter your bloodstream and then travel through your body, killing cancer cells.
Chemotherapy is sometimes recommended after surgery if there's an increased risk that the cancer might return. It can also be used before surgery to shrink the cancer so that it's more likely to be removed completely during surgery.
Chemotherapy may be recommended for treating advanced or recurrent endometrial cancer that has spread beyond the uterus.
Hormone therapy
Hormone therapy involves taking medications to lower the hormone levels in the body. In response, cancer cells that rely on hormones to help them grow might die. Hormone therapy may be an option if you have advanced endometrial cancer that has spread beyond the uterus.
Targeted drug therapy
Targeted drug treatments focus on specific weaknesses present within cancer cells. By blocking these weaknesses, targeted drug treatments can cause cancer cells to die. Targeted drug therapy is usually combined with chemotherapy for treating advanced endometrial cancer.
Immunotherapy
Immunotherapy is a drug treatment that helps your immune system to fight cancer. Your body's disease-fighting immune system might not attack cancer because the cancer cells produce proteins that blind the immune system cells. Immunotherapy works by interfering with that process. For endometrial cancer, immunotherapy might be considered if the cancer is advanced and other treatments haven't helped.
Supportive (palliative) care
Palliative care is specialized medical care that focuses on providing relief from pain and other symptoms of a serious illness. Palliative care specialists work with you, your family and your other doctors to provide an extra layer of support that complements your ongoing care. Palliative care can be used while undergoing other aggressive treatments, such as surgery, chemotherapy or radiation therapy.
When palliative care is used along with all of the other appropriate treatments, people with cancer may feel better and live longer.
Palliative care is provided by a team of doctors, nurses and other specially trained professionals. Palliative care teams aim to improve the quality of life for people with cancer and their families. This form of care is offered alongside curative or other treatments you may be receiving.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Endometrial cancer and Learn More about Diseases

Athlete's foot

Dengue fever
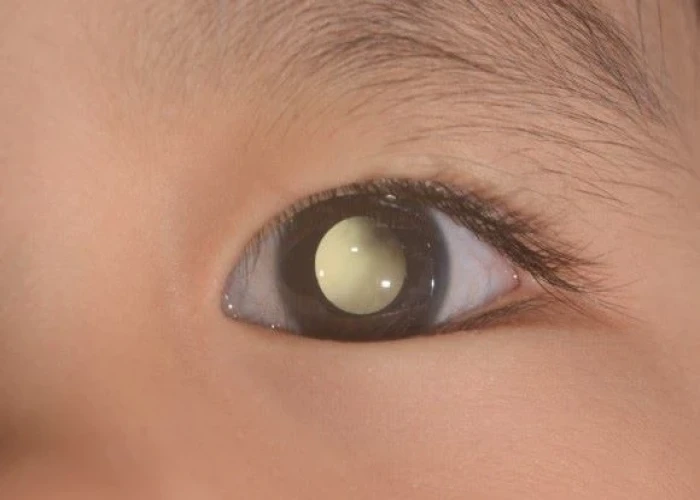
Retinoblastoma
Undifferentiated pleomorphic sarcoma
Mumps
Ampullary cancer

Pyelitis

Hyperoxaluria and oxalosis
endometrial cancer, এন্ডমেট্রিয়াল ক্যান্সার
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.