 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Epidermolysis bullosa

Epidermolysis bullosa (EB) is a rare genetic disorder that affects the skin and mucous membranes. People with EB have skin that is fragile and easily blistered, which can lead to chronic wounds, scarring, and infection. The severity of EB can vary widely, from mild blistering to life-threatening complications.
EB is caused by mutations in genes that are involved in the structure and function of the proteins that hold the layers of skin together. There are several different types of EB, each with different genetic and clinical features. The most severe form of EB is known as junctional EB, which can be fatal in infancy.
There is no cure for EB, and treatment is primarily supportive and aimed at preventing or managing complications. Treatment may include wound care, infection control, pain management, and nutritional support. In some cases, surgery may be needed to address complications such as contractures or skin cancer.
EB can have a significant impact on quality of life, and people with EB often require specialized medical care and support. Care may be provided by a team of healthcare professionals, including dermatologists, wound care specialists, nutritionists, and mental health providers. Genetic counseling may also be recommended for affected individuals and their families.
Research Papers
Disease Signs and Symptoms
- Fragile skin
- Tiny white skin bumps or pimples (milia)
- Thickened skin on the palms and soles of the feet
- Swollen (Edema)
- Itching
- Skin bumps
- Scalp blistering, scarring and hair loss (scarring alopecia)
- Hair loss
- Skin is thick
- Blisters inside the mouth and throat
- Nails thick and hard
- Blisters
- Dental problems, such as tooth decay from poorly formed enamel
Disease Causes
Epidermolysis bullosa
Epidermolysis bullosa is usually inherited. The disease gene may be passed on from one parent who has the disease (autosomal dominant inheritance). Or it may be passed on from both parents (autosomal recessive inheritance) or arise as a new mutation in the affected person that can be passed on.
The skin is made up of an outer layer (epidermis) and an underlying layer (dermis). The area where the layers meet is called the basement membrane. The various types of epidermolysis bullosa are largely defined by which layer the blisters form in.
The main types of epidermolysis bullosa are:
- Epidermolysis bullosa simplex. This is the most common form. It develops in the outer layer of skin and mainly affects the palms and the feet. The blisters usually heal without scarring.
- Junctional epidermolysis bullosa. This type may be severe, with blisters beginning in infancy. A baby with this condition may develop a hoarse-sounding cry from continual blistering and scarring of the vocal cords.
- Dystrophic epidermolysis bullosa. This type is related to a flaw in the gene that helps produce a type of collagen that provides strength to the pig-skinlike dermis layer of the skin. If this substance is missing or doesn't function, the layers of the skin won't join properly.
Disease Prevents
Epidermolysis bullosa
It's not possible to prevent epidermolysis bullosa. But you can take steps to help prevent blisters and infection.
- Handle your child gently. Your infant or child needs cuddling, but be very gentle. To pick up your child, place him or her on soft material, such as cotton, and support under the buttocks and behind the neck. Don't lift your child from under his or her arms.
- Take special care with the diaper area. If your child wears diapers, remove the elastic bands and avoid cleansing wipes. Line the diaper with a nonstick dressing or spread it with a thick layer of zinc oxide paste.
- Keep the home environment cool. Set your thermostat so that your home remains cool and the temperature remains steady.
- Keep the skin moist. Gently apply lubricants, such as petroleum jelly.
- Dress your child in soft clothes. Use soft clothing that's simple to get on and off. It may help to remove labels and put clothing on seam-side out to minimize scratching. Try sewing foam pads into the lining of clothing by elbows, knees and other pressure points. Use soft special shoes, if possible.
- Prevent scratching. Trim your child's fingernails regularly. Consider putting mittens on him or her at bedtime to help prevent scratching and infection.
- Encourage your child to be active. As your child grows, encourage him or her to be involved in activities that don't cause skin injury. Swimming is a good option. For children with mild forms of epidermolysis bullosa, they can protect their skin by wearing long pants and sleeves for outdoor activities.
- Cover hard surfaces. For example, place sheepskin on car seats and line the bathing tub with a thick towel.
Disease Treatments
If lifestyle changes and home care don't control the signs and symptoms of epidermolysis bullosa, treatments may include medications, surgery and rehabilitation. The condition often progresses despite treatment, sometimes causing serious complications and death.
Medications
Medications can help control pain and itching and treat complications such as infection in the bloodstream (sepsis). The doctor may prescribe oral antibiotics if the wounds show signs of widespread infection (fever, weakness, swollen lymph glands).
Surgery
Surgical treatment may be needed. Options sometimes used for this condition include:
- Widening the esophagus. Blistering and scarring of the esophagus may lead to esophageal narrowing, making eating difficult. Surgical dilation of the esophagus can relieve this and make it easier for food to travel from the mouth to the stomach. Risks include esophageal perforation.
- Placing a feeding tube. To improve nutrition and help with weight gain, a feeding tube (gastrostomy tube) may be implanted to deliver food directly to the stomach.
- Grafting skin. If scarring has affected the function of the hand, the doctor may suggest a skin graft.
- Restoring mobility. Repeated blistering and scarring can cause fusing of the fingers or toes or abnormal bends in the joints (contractures). The doctor may recommend surgery to correct these conditions, particularly if they interfere with normal motion.
Rehabilitation therapy
Working with a rehabilitation specialist (physical therapist, occupational therapist) can help ease the limitations on motion caused by scarring and contractures.
Potential future treatments
Researchers are studying better ways to treat and relieve the symptoms of epidermolysis bullosa, including:
- Gene therapy
- Bone marrow (stem cell) transplantation
- Protein replacement therapies
- Cell-based therapies
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Epidermolysis bullosa and Learn More about Diseases
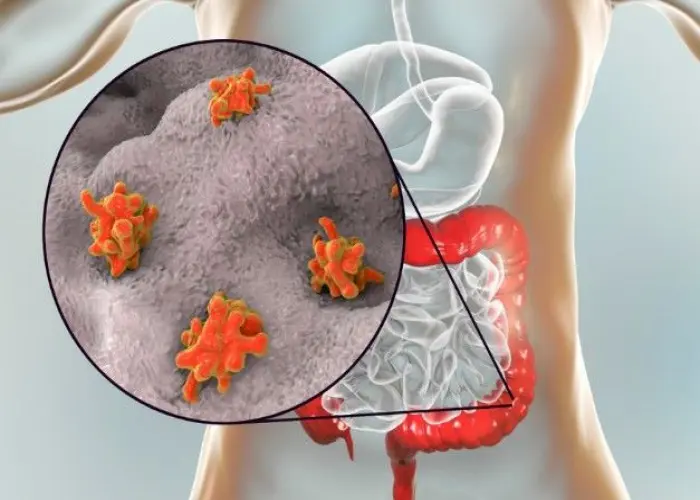
Amoebic Dysentry
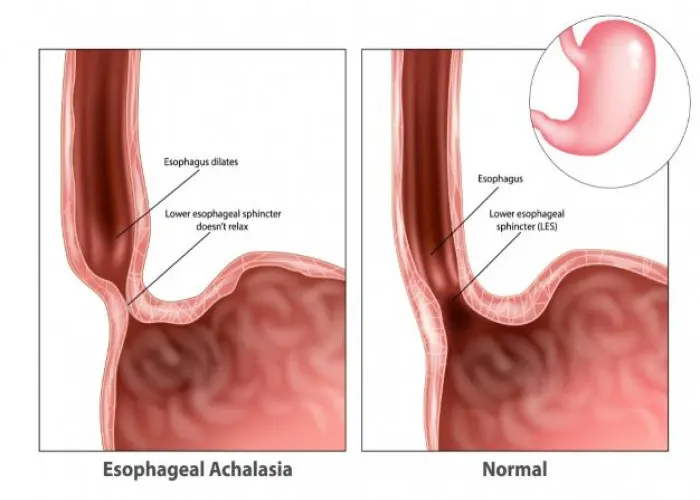
Achalasia

Posterior vaginal prolapse (Rectocele)
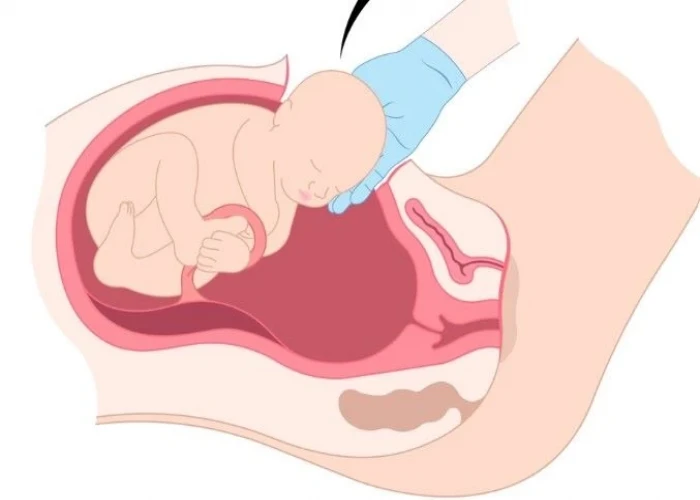
Postpartum preeclampsia

Schizotypal personality disorder

Male infertility
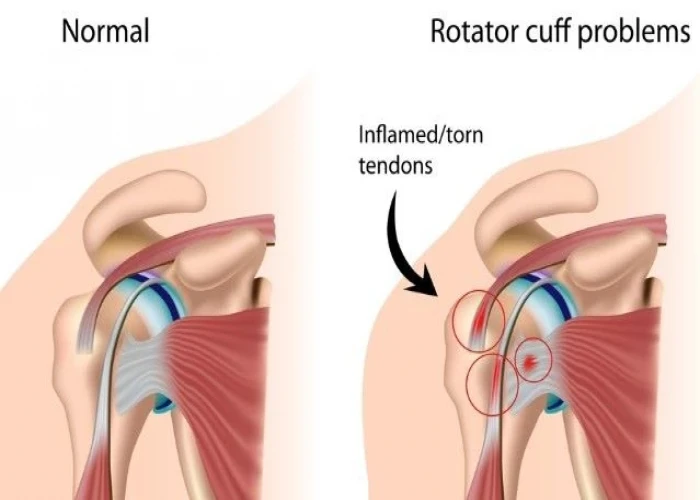
Rotator cuff injury

Pubic lice (crabs)
epidermolysis bullosa, এপিডার্মোলাইসেস বুলোসা
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
