 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Renal transplant - Generics
Renal transplantation is a surgical procedure that involves the replacement of a diseased or non-functional kidney with a healthy kidney from a donor. The procedure is typically performed on patients with end-stage renal disease, a condition in which the kidneys can no longer function properly, and dialysis is required to filter waste products from the blood.
Renal transplantation offers several benefits over dialysis, including improved quality of life, longer life expectancy, and reduced healthcare costs. The success of a renal transplant depends on several factors, including the health of the donor and recipient, compatibility of the donor's kidney with the recipient's immune system, and the quality of the medical care received after the surgery.
The transplantation process involves several stages, including evaluation and selection of a suitable donor, pre-transplant testing and preparation of the recipient, the surgical procedure itself, and post-transplant care and monitoring. The surgery typically lasts several hours and involves the removal of the diseased kidney and implantation of the new kidney.
After the surgery, the recipient will need to take immunosuppressive medications to prevent rejection of the new kidney by the body's immune system. These medications can have side effects and require careful monitoring to ensure they are effective and safe.
Renal transplantation is generally considered a safe and effective treatment for end-stage renal disease, and most patients experience improved quality of life and increased life expectancy after the surgery. However, there are risks associated with the procedure, including complications related to surgery, infection, and rejection of the new kidney. Close monitoring and follow-up care are essential for the long-term success of the transplant.

Bleeding or blood clottin...

Uterine hemorrhage

Rocky Mountain spotted fe...
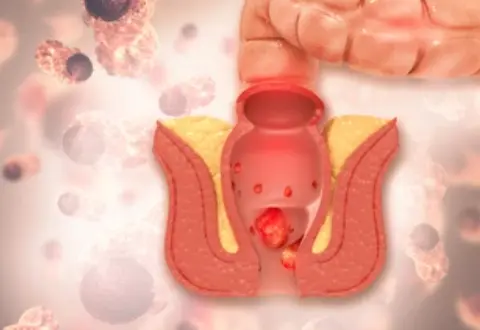
Haemorrhoids (piles)

Generalized tonic-clonic...

Rickets

Electrolyte replenisher

Folliculitis
Renal transplant, রেনাল ট্রান্সপ্ল্যান্ট
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.