Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Vaginal agenesis
Vaginal agenesis, also known as Mayer-Rokitansky-Küster-Hauser syndrome, is a rare congenital condition where the vagina does not develop properly or is absent. This can occur in varying degrees, ranging from a shortened or narrowed vagina to a complete absence of the vagina.
The exact cause of vaginal agenesis is not well understood, but it is thought to be related to abnormalities in embryonic development. In some cases, vaginal agenesis may occur in conjunction with other developmental abnormalities or genetic disorders.
Symptoms of vaginal agenesis may include primary amenorrhea, which is the absence of menstruation, difficulty with sexual intercourse, and pelvic pain. Diagnosis of vaginal agenesis typically involves a pelvic exam, imaging tests such as ultrasound, MRI, or CT scan, and in some cases genetic testing.
Treatment options for vaginal agenesis depend on the severity of the condition and may include dilation of the vagina using special devices, surgical creation of a new vagina, or the use of a vaginal prosthesis or grafting. In some cases, hormone therapy may also be used to help support the development of secondary sexual characteristics.
While vaginal agenesis can be a difficult and distressing condition, with proper diagnosis and treatment, women can lead healthy and fulfilling lives. It is important to discuss treatment options with a healthcare provider and to seek support from counselors or support groups if needed.
Research Papers
Disease Signs and Symptoms
- Abdomen pain
- Abdomen cramps
- Hearing problems or deafness
- Undeveloped vagina
Disease Causes
Vaginal agenesis
It's not clear what causes vaginal agenesis, but at some point during the first 20 weeks of pregnancy, tubes called the mullerian ducts don't develop properly.
Typically, the lower portion of these ducts develops into the uterus and vagina, and the upper portion becomes the fallopian tubes. The underdevelopment of the mullerian ducts results in an absent or partially closed vagina, absent or partial uterus, or both.
Disease Prevents
Disease Treatments
Treatment for vaginal agenesis often occurs in the late teens or early 20s, but you may wait until you're older and you feel motivated and ready to participate in treatment.
You and your health care provider can discuss treatment options. Depending on your individual condition, options may involve no treatment or creating a vagina by self-dilation or surgery.
Self-dilation
Self-dilation is typically recommended as the first option. Self-dilation may allow you to create a vagina without surgery. The goal is to lengthen the vagina to a size comfortable for sexual intercourse.
During self-dilation, you press a small, round rod (dilator) — similar to a firm tampon — against your skin at your vaginal opening or inside your existing vagina for 10 to 30 minutes 1 to 3 times a day. As the weeks go by, you switch to larger dilators. It may take a few months to get the result you want.
Discuss the process of self-dilation with your health care provider so that you know what to do and talk about dilator options to find what works best for you. Using self-dilation at intervals recommended by your health care provider or having frequent sexual intercourse is needed over time to maintain the length of your vagina.
Some patients report problems with urinating and with vaginal bleeding and pain, especially in the beginning. Artificial lubrication and trying a different type of dilator may be helpful. Your skin stretches more easily after a warm bath so that may be a good time for dilation.
Vaginal dilation through frequent intercourse is an option for self-dilation for women who have willing partners. If you'd like to give this method a try, talk to your health care provider about the best way to proceed.
Surgery
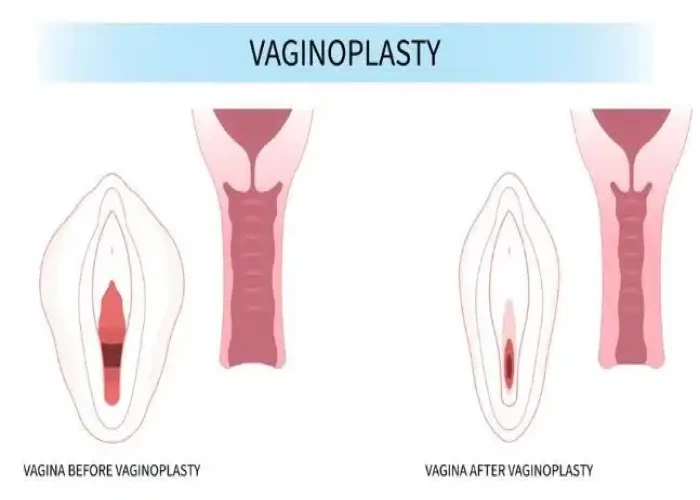
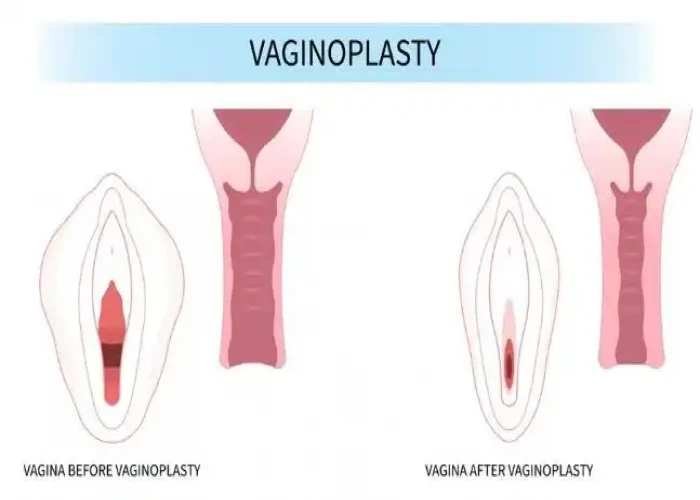
If self-dilation doesn't work, surgery to create a functional vagina (vaginoplasty) may be an option. Types of vaginoplasty surgery include:
- Using a tissue graft. Your surgeon may choose from a variety of grafts using your own tissue to create a vagina. Possible sources include skin from the outer thigh, buttocks or lower abdomen.
- Your surgeon makes an incision to create the vaginal opening, places the tissue graft over a mold to create the vagina and places it in the newly formed canal. The mold remains in place about one week.
- Generally, after surgery you keep the mold or a vaginal dilator in place but can remove it when you use the bathroom or have sexual intercourse. After the initial time recommended by your surgeon, you'll use the dilator only at night. Sexual intercourse with artificial lubrication and occasional dilation helps you maintain a functional vagina.
- Inserting a medical traction device. Your surgeon places an olive-shaped device (Vecchietti procedure) or a balloon device (balloon vaginoplasty) at your vaginal opening. Using a thin, lighted viewing instrument (laparoscope) as a guide, the surgeon connects the device to a separate traction device on your lower abdomen or through your navel.
- You tighten the traction device every day, gradually pulling the device inward to create a vaginal canal over about a week. After the device is removed, you'll use a mold of varying sizes for about three months. After three months, you may use further self-dilation or have regular sexual intercourse to maintain a functional vagina. Sexual intercourse will likely require artificial lubrication.
- Using a portion of your colon (bowel vaginoplasty). In a bowel vaginoplasty, the surgeon moves a portion of your colon to an opening in your genital area, creating a new vagina. Your surgeon then reconnects your remaining colon. You won't have to use a vaginal dilator every day after this surgery, and you're less likely to need artificial lubrication for sexual intercourse.
After surgery, use of a mold, dilation or frequent sexual intercourse is needed to maintain a functional vagina. Health care providers usually delay surgical treatments until you feel prepared and able to handle self-dilation. Without regular dilation, the newly created vaginal canal can quickly narrow and shorten, so being emotionally mature and ready to comply with aftercare is critically important.
Talk to your health care provider about the best surgical option to meet your needs, and the risks and required care after surgery.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Vaginal agenesis and Learn More about Diseases

Leukoplakia

Metatarsalgia

Pulmonary embolism

Ascites

Ruptured spleen

Pemphigus

Chronic traumatic encephalopathy

Focal segmental glomerulosclerosis (FSGS)
vaginal agenesis, ভ্যাজাইনাল এজেনেসিস, যোনি অজেনেসিস
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.