Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Traveler's diarrhea
Traveler's diarrhea is a common condition that affects people who travel to countries with inadequate sanitation and hygiene practices. It is caused by consuming food or water that has been contaminated with bacteria, viruses, or parasites.
Symptoms of traveler's diarrhea typically include abdominal cramps, nausea, and frequent, loose bowel movements. In some cases, the diarrhea may be accompanied by fever and vomiting. Most cases of traveler's diarrhea are self-limited and resolve within a few days to a week, but in some cases, the symptoms may be more severe or prolonged.
Prevention strategies for traveler's diarrhea include avoiding high-risk foods and beverages such as tap water, raw or undercooked meat or seafood, and fresh produce that may have been washed with contaminated water. Other prevention strategies include practicing good hygiene, such as frequent hand washing, and using oral rehydration solutions to prevent dehydration.
In cases of traveler's diarrhea, treatment may include anti-diarrheal medications, such as loperamide, to relieve symptoms, as well as antibiotics in certain cases. It is important to consult with a healthcare provider before taking any medications, as some may not be appropriate for all individuals or may interact with other medications.
If symptoms are severe or prolonged, or if there are signs of dehydration such as decreased urine output, dry mouth, or dizziness, it is important to seek medical attention promptly.
Research Papers
Disease Signs and Symptoms
- Loose watery stools
- Abdomen pain
- Abdomen cramps
- Nausea or vomiting
- Fever
- Diarrhea
- Black, tarry or bloody stools
- Abrupt onset of passage of three or more loose stools a day
- Blood in stool
Disease Causes
Traveler's diarrhea
It's possible that traveler's diarrhea may stem from the stress of traveling or a change in diet. But usually infectious agents — such as bacteria, viruses or parasites — are to blame. You typically develop traveler's diarrhea after ingesting food or water contaminated with organisms from feces.
So why aren't natives of high-risk countries affected in the same way? Often their bodies have become accustomed to the bacteria and have developed immunity to them.
Disease Prevents
Traveler's diarrhea
Watch what you eat
The general rule of thumb when traveling to another country is this: Boil it, cook it, peel it or forget it. But, it's still possible to get sick even if you follow these rules.
Other tips that may help decrease your risk of getting sick include:
- Don't consume food from street vendors.
- Avoid unpasteurized milk and dairy products, including ice cream.
- Avoid raw or undercooked meat, fish and shellfish.
- Steer clear of moist food at room temperature, such as sauces and buffet offerings.
- Eat foods that are well cooked and served hot.
- Stick to fruits and vegetables that you can peel yourself, such as bananas, oranges and avocados. Stay away from salads and from fruits you can't peel, such as grapes and berries.
- Be aware that alcohol in a drink won't keep you safe from contaminated water or ice.
Don't drink the water
When visiting high-risk areas, keep the following tips in mind:
- Avoid unsterilized water — from tap, well or stream. If you need to consume local water, boil it for three minutes. Let the water cool naturally and store it in a clean covered container.
- Avoid locally made ice cubes or mixed fruit juices made with tap water.
- Beware of sliced fruit that may have been washed in contaminated water.
- Use bottled or boiled water to mix baby formula.
- Order hot beverages, such as coffee or tea, and make sure they're steaming hot.
- Feel free to drink canned or bottled drinks in their original containers — including water, carbonated beverages, beer or wine — as long as you break the seals on the containers yourself. Wipe off any can or bottle before drinking or pouring.
- Use bottled water to brush your teeth.
- Don't swim in water that may be contaminated.
- Keep your mouth closed while showering.
If it's not possible to buy bottled water or boil your water, bring some means to purify water. Consider a water-filter pump with a microstrainer filter that can filter out small microorganisms.
You can also chemically disinfect water with iodine or chlorine. Iodine tends to be more effective, but is best reserved for short trips, as too much iodine can be harmful to your system. You can purchase water-disinfecting tablets containing chlorine, iodine tablets or crystals, or other disinfecting agents at camping stores and pharmacies. Be sure to follow the directions on the package.
Follow additional tips
Here are other ways to reduce your risk of traveler's diarrhea:
- Make sure dishes and utensils are clean and dry before using them.
- Wash your hands often and always before eating. If washing isn't possible, use an alcohol-based hand sanitizer with at least 60% alcohol to clean your hands before eating.
- Seek out food items that require little handling in preparation.
- Keep children from putting things — including their dirty hands — in their mouths. If possible, keep infants from crawling on dirty floors.
- Tie a colored ribbon around the bathroom faucet to remind you not to drink — or brush your teeth with — tap water.
Other preventive measures
Public health experts generally don't recommend taking antibiotics to prevent traveler's diarrhea, because doing so can contribute to the development of antibiotic-resistant bacteria.
Antibiotics provide no protection against viruses and parasites, but they can give travelers a false sense of security about the risks of consuming local foods and beverages. They can also cause unpleasant side effects, such as skin rashes, skin reactions to the sun and vaginal yeast infections.
As a preventive measure, some doctors suggest taking bismuth subsalicylate, which has been shown to decrease the likelihood of diarrhea. However, don't take this medication for longer than three weeks, and don't take it at all if you're pregnant or allergic to aspirin. Talk to your doctor before taking bismuth subsalicylate if you're taking certain medications, such as anticoagulants.
Common harmless side effects of bismuth subsalicylate include a black-colored tongue and dark stools. In some cases, it can cause constipation, nausea and, rarely, ringing in your ears (tinnitus).
Disease Treatments
Traveler's diarrhea may get better without any treatment. But while you're waiting, it's important to try to stay hydrated with safe liquids, such as bottled water or water with electrolytes such as an oral rehydration solution (see below). If you don't seem to be improving quickly, several medications are available to help relieve symptoms.
- Anti-motility agents. These medications — which include loperamide and drugs containing diphenoxylate — provide prompt but temporary relief by reducing muscle spasms in your gastrointestinal tract, slowing the transit time through your digestive system and allowing more time for absorption.
- Anti-motility medications aren't recommended for infants or people with a fever or bloody diarrhea, as they can delay clearance of the infectious organisms and make the illness worse.
- Also, stop using anti-motility agents after 48 hours if you have abdominal pain or if your signs or symptoms worsen and your diarrhea continues. In such cases, see a doctor. You may need blood or stool tests and treatment with an antibiotic.
- Bismuth subsalicylate. This over-the-counter medication can decrease the frequency of your stools and shorten the duration of your illness. However, it isn't recommended for children, pregnant women or people who are allergic to aspirin.
- Antibiotics. If you have more than four loose stools a day or severe symptoms, including a fever or blood, pus or mucus in your stools, a doctor may prescribe a course of antibiotics.
Before you leave for your trip, talk to your doctor about taking a prescription with you in case you get a serious bout of traveler's diarrhea.
Avoiding dehydration
Dehydration is the most likely complication of traveler's diarrhea, so it's important to try to stay well hydrated.
An oral rehydration salts (ORS) solution is the best way to replace lost fluids. These solutions contain water and salts in specific proportions to replenish both fluids and electrolytes. They also contain glucose to enhance absorption in the intestinal tract.
Bottled oral rehydration products are available in drugstores in developed areas, and many pharmacies carry their own brands. You can find packets of powdered oral rehydration salts, labeled World Health Organization (WHO)-ORS, at stores, pharmacies and health agencies in most countries. Reconstitute the powder in bottled or boiled water according to the directions on the package.
If these products are unavailable, you can prepare your own rehydrating solution in an emergency by mixing together:
- 3/4 teaspoon table salt
- 2 tablespoons sugar
- 1 quart uncontaminated bottled or boiled water
- Sugar-free flavor powder, such as Crystal Light (optional)
You or your child can drink the solution in small amounts throughout the day as a supplement to solid foods or formula, as long as dehydration persists. Small amounts reduce the likelihood of vomiting. Breastfed infants also can drink the solution but should continue nursing on demand.
If dehydration symptoms — such as dry mouth, intense thirst, little or no urination, dizziness, or extreme weakness — don't improve, seek medical care right away. Oral rehydration solutions are intended only for urgent short-term use.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Traveler's diarrhea and Learn More about Diseases

Autism spectrum disorder

Anthrax
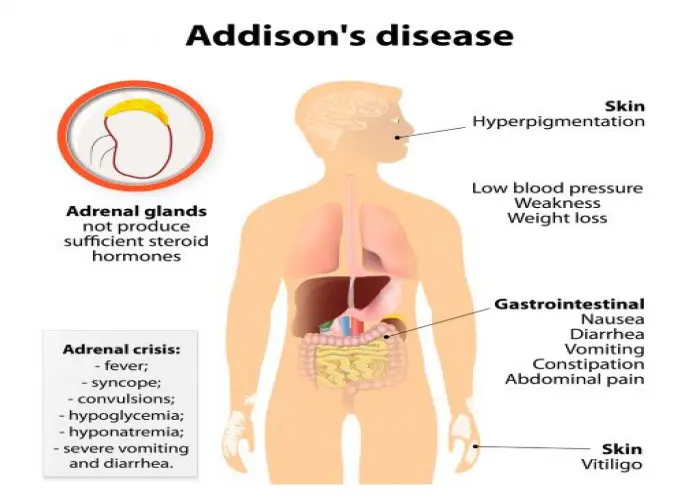
Addison's disease

Flatfeet
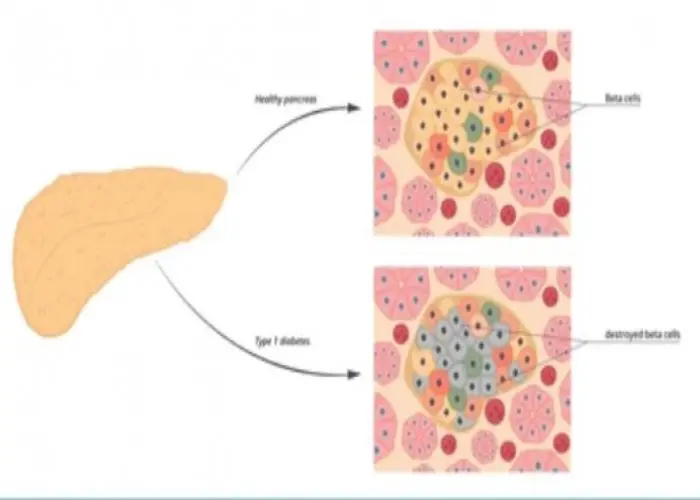
Autoimmune pancreatitis

Dysphagia

Rectal prolapse

Milk allergy
traveler's diarrhea, যাত্রীর ডায়রিয়া
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.