 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Spina bifida

Spina bifida is a birth defect that affects the spine and spinal cord. It occurs when the neural tube, which is the structure that forms the brain and spinal cord, does not close completely during fetal development. This can lead to a range of physical and neurological problems.
The severity of spina bifida can vary widely, depending on the location and size of the spinal opening. The most severe form of spina bifida is called myelomeningocele, in which the spinal cord and surrounding tissues protrude through an opening in the spine. This can cause paralysis, weakness, and other neurological problems.
Other types of spina bifida include meningocele, in which only the meninges, or protective covering of the spinal cord, protrude through the opening, and spina bifida occulta, which is the mildest form of spina bifida and may not cause any noticeable symptoms.
There is no cure for spina bifida, but treatments such as surgery, physical therapy, and medications can help manage symptoms and improve quality of life. Surgery is typically recommended for infants with myelomeningocele to repair the spinal opening and prevent further damage to the spinal cord. Physical therapy can help improve mobility and prevent complications such as contractures or scoliosis. In some cases, medications such as antibiotics or shunts may be necessary to manage associated conditions such as infections or hydrocephalus.
The exact cause of spina bifida is not well understood, but it is thought to be related to a combination of genetic and environmental factors. Certain risk factors, such as a family history of spina bifida, maternal obesity or uncontrolled diabetes, and certain medications, may increase the risk of spina bifida.
With appropriate treatment and care, many people with spina bifida are able to lead full and productive lives. It is important for individuals with spina bifida to receive ongoing medical care and support to manage symptoms and prevent complications.
Research Papers
Disease Signs and Symptoms
- Genetic problems
- Bone pain
Disease Causes
Spina bifida
Doctors aren't certain what causes spina bifida. It's thought to result from a combination of genetic, nutritional and environmental risk factors, such as a family history of neural tube defects and folate (vitamin B-9) deficiency.
Disease Prevents
Spina bifida
Folic acid, taken in supplement form starting at least one month before conception and continuing through the first trimester of pregnancy, greatly reduces the risk of spina bifida and other neural tube defects.
Get folic acid first
Having enough folic acid in your system by the early weeks of pregnancy is critical to prevent spina bifida. Because many women don't discover that they're pregnant until this time, experts recommend that all women of childbearing age take a daily supplement of 400 micrograms (mcg) of folic acid.
Several foods are fortified with 400 mcg of folic acid per serving, including:
- Enriched bread
- Pasta
- Rice
- Some breakfast cereals
Folic acid may be listed on food packages as folate, which is the natural form of folic acid found in foods.
Planning pregnancy
Adult women who are planning pregnancy or who could become pregnant should be advised to get 400 to 800 mcg of folic acid a day.
Your body doesn't absorb folate as easily as it absorbs synthetic folic acid, and most people don't get the recommended amount of folate through diet alone, so vitamin supplements are necessary to prevent spina bifida. And it's possible that folic acid will also help reduce the risk of other birth defects, including cleft lip, cleft palate and some congenital heart defects.
It's also a good idea to eat a healthy diet, including foods rich in folate or enriched with folic acid. This vitamin is present naturally in many foods, including:
- Beans and peas
- Citrus fruits and juices
- Egg yolks
- Milk
- Avocados
- Dark green vegetables, such as broccoli and spinach
When higher doses are needed
If you have spina bifida or if you've previously given birth to a child with spina bifida, you'll need extra folic acid before you become pregnant. If you're taking anti-seizure medications or you have diabetes, you may also benefit from a higher dose of this B vitamin. Check with your doctor before taking additional folic acid supplements.
Disease Treatments
Spina bifida treatment depends on the severity of the condition. Spina bifida occulta often doesn't require any treatment at all, but other types of spina bifida do.
Surgery before birth
Nerve function in babies with spina bifida can worsen after birth if spina bifida isn't treated. Prenatal surgery for spina bifida (fetal surgery) takes place before the 26th week of pregnancy. Surgeons expose the pregnant mother's uterus surgically, open the uterus and repair the baby's spinal cord. In select patients, this procedure can be performed less invasively with a special surgical tool (fetoscope) inserted into the uterus.
Research suggests that children with spina bifida who had fetal surgery may have reduced disability and be less likely to need crutches or other walking devices. Fetal surgery may also reduce the risk of hydrocephalus. Ask your doctor whether this procedure may be appropriate for you. Discuss the potential benefits and risks, such as possible premature delivery and other complications, for you and your baby.
It's important to have a comprehensive evaluation to determine whether fetal surgery is feasible. This specialized surgery should only be done at a health care facility that has experienced fetal surgery experts, a multispecialty team approach and neonatal intensive care. Typically the team includes a fetal surgeon, pediatric neurosurgeon, maternal-fetal medicine specialist, fetal cardiologist and neonatologist.
Cesarean birth
Many babies with myelomeningocele tend to be in a feet-first (breech) position. If your baby is in this position or if your doctor has detected a large cyst or sac, cesarean birth may be a safer way to deliver your baby.
Surgery after birth
Myelomeningocele requires surgery to close the opening in the baby's back within 72 hours of birth. Performing the surgery early can help minimize the risk of infection associated with the exposed nerves. It may also help protect the spinal cord from more trauma.
During the procedure, a neurosurgeon places the spinal cord and exposed tissue inside the baby's body and covers them with muscle and skin. At the same time, the neurosurgeon may place a shunt in the baby's brain to control hydrocephalus.
Treatment for complications
In babies with myelomeningocele, irreparable nerve damage has likely already occurred and ongoing care from a multispecialty team of surgeons, physicians and therapists is usually needed. Babies with myelomeningocele may need more surgery for a variety of complications. Treatment for complications — such as weak legs, bladder and bowel problems, or hydrocephalus — typically begins soon after birth.
Depending on the severity of spina bifida and the complications, treatment options may include:
- Walking and mobility aids. Some babies may start exercises to prepare their legs for walking with braces or crutches when they're older. Some children may need walkers or a wheelchair. Mobility aids, along with regular physical therapy, can help a child become independent. Even children who need a wheelchair can learn to function very well and become self-sufficient.
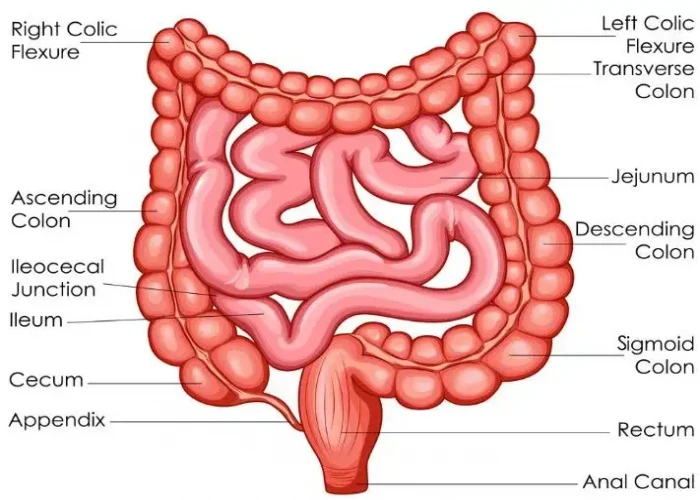
- Bowel and bladder management. Routine bowel and bladder evaluations and management plans help reduce the risk of organ damage and illness. Evaluations include X-rays, kidney scans, ultrasounds, blood tests and bladder function studies. These evaluations will be more frequent in the first few years of life but less often as children grow. A specialist in pediatric urology with experience in evaluating and performing surgery on children with spina bifida may offer the most effective management options.
- Bowel management may include oral medications, suppositories, enemas, surgery or a combination of these approaches.
- Bladder management may include medications, using catheters to empty the bladder, surgery or a combination of treatments.
- Surgery for hydrocephalus. Most babies with myelomeningocele will need a surgically placed tube that allows fluid in the brain to drain into the abdomen (ventricular shunt). This tube might be placed just after birth, during the surgery to close the sac on the lower back or later as fluid accumulates. A less invasive procedure, called endoscopic third ventriculostomy, may be an option. But candidates must be carefully chosen and meet certain criteria. During the procedure, the surgeon uses a small video camera to see inside the brain and makes a hole in the bottom of or between the ventricles so cerebrospinal fluid can flow out of the brain.
- Treatment and management of other complications. Special equipment such as bath chairs, commode chairs and standing frames may help with daily functioning. Whatever the issue — orthopedic complications, tethered spinal cord, GI issues, skin problems or others — most spina bifida complications can be treated or at least managed to improve quality of life.
Ongoing care
Children with spina bifida need close follow-up care and observation. Their primary care doctors evaluate growth, the need for vaccinations and general medical issues, and they coordinate medical care.
Children with spina bifida also often need treatment and ongoing care from:
- Physical medicine and rehabilitation
- Neurology
- Neurosurgery
- Urology
- Orthopedics
- Physical therapy
- Occupational therapy
- Special education teachers
- Social workers
- Dietitians
Parents and other caregivers are a key part of the team. They can learn how to help manage a child's condition and how to encourage and support the child emotionally and socially.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Spina bifida and Learn More about Diseases
Small bowel prolapse (enterocele)

Myocarditis

Carcinoid tumors

Gonorrhea

Hantavirus pulmonary syndrome
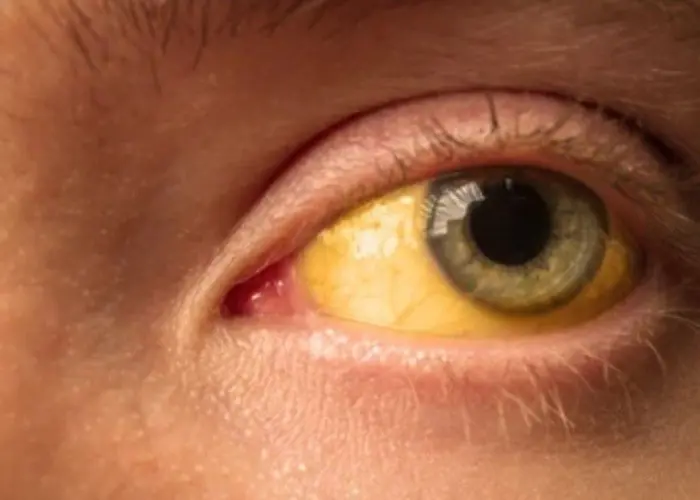
Cirrhosis

Blocked tear duct

High blood pressure in children
spina bifida, স্পিনা বিফিদা
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
