 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
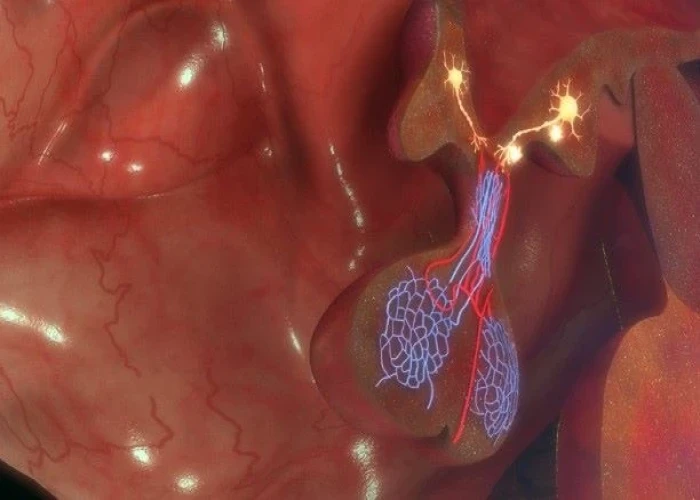
Pulmonary embolism

A pulmonary embolism (PE) is a serious medical condition in which a blood clot forms in one of the pulmonary arteries, which are the blood vessels that carry blood from the heart to the lungs. When a clot blocks a pulmonary artery, it can cause decreased blood flow to the lungs and reduce the amount of oxygen in the blood. This can lead to symptoms such as shortness of breath, chest pain, coughing up blood, and a rapid or irregular heartbeat.
Pulmonary embolisms most commonly occur as a result of deep vein thrombosis (DVT), a condition in which blood clots form in the deep veins of the legs or other parts of the body. These clots can break free and travel to the lungs, causing a PE.
Risk factors for pulmonary embolism include prolonged immobility, recent surgery or injury, cancer, pregnancy, smoking, and certain medical conditions such as heart failure or clotting disorders.
Treatment for pulmonary embolism typically involves blood thinning medications, such as heparin or warfarin, to help dissolve the clot and prevent the formation of new clots. In severe cases, procedures such as thrombolysis, where medication is injected directly into the clot to dissolve it, or embolectomy, where a catheter is used to remove the clot, may be necessary.
Prompt diagnosis and treatment of pulmonary embolism is important, as it can be a life-threatening condition. If you are experiencing symptoms of pulmonary embolism, such as sudden shortness of breath, chest pain, or coughing up blood, seek medical attention immediately.
Research Papers
Disease Signs and Symptoms
- Shortness of breath (dyspnea)
- Chest pain
- Cough
- Irregular heartbeats (arrhythmia)
- Dizziness, lightheadedness or faintness
- Dizziness (vertigo)
- Excessive sweat
- Fever
- Leg pain
Disease Causes
Pulmonary embolism
Pulmonary embolism occurs when a clump of material, most often a blood clot, gets wedged into an artery in your lungs. These blood clots most commonly come from the deep veins of your legs, a condition known as deep vein thrombosis (DVT).
In many cases, multiple clots are involved in pulmonary embolism. The portions of lung served by each blocked artery are robbed of blood and may die. This is known as pulmonary infarction. This makes it more difficult for your lungs to provide oxygen to the rest of your body.
Occasionally, blockages in the blood vessels are caused by substances other than blood clots, such as:
- Fat from the marrow of a broken long bone
- Part of a tumor
- Air bubbles
Disease Prevents
Pulmonary embolism
Preventing clots in the deep veins in your legs (deep vein thrombosis) will help prevent pulmonary embolism. For this reason, most hospitals are aggressive about taking measures to prevent blood clots, including:
- Blood thinners (anticoagulants). These medications are often given to people at risk of clots before and after an operation — as well as to people admitted to the hospital with medical conditions, such as heart attack, stroke or complications of cancer.
- Compression stockings. Compression stockings steadily squeeze your legs, helping your veins and leg muscles move blood more efficiently. They offer a safe, simple and inexpensive way to keep blood from stagnating during and after general surgery.
- Leg elevation. Elevating your legs when possible and during the night also can be very effective. Raise the bottom of your bed 4 to 6 inches (10 to 15 cm) with blocks or books.
- Physical activity. Moving as soon as possible after surgery can help prevent pulmonary embolism and hasten recovery overall. This is one of the main reasons your nurse may push you to get up, even on your day of surgery, and walk despite pain at the site of your surgical incision.
- Pneumatic compression. This treatment uses thigh-high or calf-high cuffs that automatically inflate with air and deflate every few minutes to massage and squeeze the veins in your legs and improve blood flow.
Prevention while traveling
The risk of blood clots developing while traveling is low, but increases as long-haul travel increases. If you have risk factors for blood clots and you're concerned about travel, talk with your doctor.
Your doctor might suggest the following to help prevent blood clots during travel:
- Drink plenty of fluids. Water is the best liquid for preventing dehydration, which can contribute to the development of blood clots. Avoid alcohol, which contributes to fluid loss.
- Take a break from sitting. Move around the airplane cabin once an hour or so. If you're driving, stop every so often and walk around the car a couple of times. Do a few deep knee bends.
- Fidget in your seat. Flex your ankles every 15 to 30 minutes.
- Wear support stockings. Your doctor may recommend these to help promote circulation and fluid movement in your legs. Compression stockings are available in a range of stylish colors and textures. There are even devices, called stocking butlers, to help you put on the stockings.
Disease Treatments
Treatment of pulmonary embolism is aimed at keeping the blood clot from getting bigger and preventing new clots from forming. Prompt treatment is essential to prevent serious complications or death.
Medications
Medications include different types of blood thinners and clot dissolvers.
- Blood thinners (anticoagulants). These drugs prevent existing clots from enlarging and new clots from forming while your body works to break up the clots. Heparin is a frequently used anticoagulant that can be given through the vein or injected under the skin. It acts quickly and is often overlapped for several days with an oral anticoagulant, such as warfarin, until it becomes effective, which can take days.
- Newer oral anticoagulants work more quickly and have fewer interactions with other medications. Some have the advantage of being given by mouth, without the need for overlap with heparin. However, all anticoagulants have side effects, and bleeding is the most common.
- Clot dissolvers (thrombolytics). While clots usually dissolve on their own, sometimes thrombolytics given through the vein can dissolve clots quickly. Because these clot-busting drugs can cause sudden and severe bleeding, they usually are reserved for life-threatening situations.
Surgical and other procedures
- Clot removal. If you have a very large, life-threatening clot in your lung, your doctor may suggest removing it via a thin, flexible tube (catheter) threaded through your blood vessels.
- Vein filter. A catheter can also be used to position a filter in the body's main vein (inferior vena cava) that leads from your legs to the right side of your heart. This filter can help keep clots from going to your lungs. This procedure is typically reserved for people who can't take anticoagulant drugs or when they have had recurrent clots despite use of anticoagulants. Some filters can be removed when no longer needed.
Ongoing care
Because you may be at risk of another deep vein thrombosis or pulmonary embolism, it's important to continue treatment, such as remaining on blood thinners, and be monitored as often as suggested by your doctor. Also, keep regular doctor visits to prevent or treat complications.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Pulmonary embolism and Learn More about Diseases

Perimenopause

Nicotine dependence

Wheat allergy

Conjoined twins
Pituitary tumors

Spontaneous coronary artery dissection (SCAD)

Vitiligo (Leucoderma)

Trigger finger
pulmonary embolism, পালমোনারি ইমবোলিসম
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
