 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Psoriasis

Psoriasis is a chronic skin condition that causes the skin cells to multiply faster than normal, resulting in the formation of raised, scaly, and itchy patches on the skin. The condition is thought to be caused by a combination of genetic and environmental factors, and it is not contagious.
The symptoms of psoriasis can vary in severity and can be different for each person, but typically include red, raised patches of skin that are covered in silvery scales, itching, dry or cracked skin, and thickened or pitted nails. Psoriasis can affect any part of the body, but is most commonly found on the scalp, elbows, knees, and lower back.
There is no cure for psoriasis, but there are a variety of treatments available that can help to manage the symptoms. Treatment options include topical medications such as corticosteroids and vitamin D analogues, phototherapy (light therapy), and oral medications such as retinoids and immunosuppressants. In severe cases, biologic medications that target specific parts of the immune system may be used.
In addition to medical treatments, there are lifestyle changes that can help to manage psoriasis symptoms, such as avoiding triggers like stress, alcohol, and certain medications, maintaining a healthy weight, and avoiding skin injuries and infections.
While psoriasis is not curable, with proper management and treatment, most people with the condition are able to manage their symptoms and lead a normal life. However, it is important to work with a healthcare professional to develop an individualized treatment plan, as the best approach will depend on the severity and location of the psoriasis, as well as the person's overall health and lifestyle.
Research Papers
Disease Signs and Symptoms
- Raised, red patches of skin (hives)
- Dry skin
- Itching
- Skin pain or burning sensation
- Nails thick and hard
- Swollen joint
- Small scaling spots (commonly seen in children)
- Dry, cracked skin that may bleed or itch
Disease Causes
Psoriasis
Psoriasis is thought to be an immune system problem that causes the skin to regenerate at faster than normal rates. In the most common type of psoriasis, known as plaque psoriasis, this rapid turnover of cells results in scales and red patches.
Just what causes the immune system to malfunction isn't entirely clear. Researchers believe both genetics and environmental factors play a role. The condition is not contagious.
Psoriasis triggers
Many people who are predisposed to psoriasis may be free of symptoms for years until the disease is triggered by some environmental factor. Common psoriasis triggers include:
- Infections, such as strep throat or skin infections
- Weather, especially cold, dry conditions
- Injury to the skin, such as a cut or scrape, a bug bite, or a severe sunburn
- Stress
- Smoking and exposure to secondhand smoke
- Heavy alcohol consumption
- Certain medications — including lithium, high blood pressure medications and antimalarial drugs
- Rapid withdrawal of oral or systemic corticosteroids
Disease Prevents
Disease Treatments
Psoriasis treatments aim to stop skin cells from growing so quickly and to remove scales. Options include creams and ointments (topical therapy), light therapy (phototherapy), and oral or injected medication.
Which treatments you use depends on how severe the psoriasis is and how responsive it has been to previous treatment. You might need to try different drugs or a combination of treatments before you find an approach that works for you. Usually, however, the disease returns.
Topical therapy
- Corticosteroids. These drugs are the most frequently prescribed medications for treating mild to moderate psoriasis. They are available as ointments, creams, lotions, gels, foams, sprays and shampoos. Mild corticosteroid ointments (hydrocortisone) are usually recommended for sensitive areas, such as your face or skin folds, and for treating widespread patches. Topical corticosteroids might be applied once a day during flares, and on alternate days or weekends only to maintain remission.
- Your doctor may prescribe a stronger corticosteroid cream or ointment— triamcinolone (Acetonide, Trianex), clobetasol (Temovate) for smaller, less-sensitive or tougher-to-treat areas.
- Long-term use or overuse of strong corticosteroids can thin the skin. Over time, topical corticosteroids may stop working.
- Vitamin D analogues. Synthetic forms of vitamin D, such as calcipotriene and calcitriol (Vectical) slow skin cell growth. This type of drug may be used alone or with topical corticosteroids. Calcitriol may cause less irritation in sensitive areas. Calcipotriene and calcitriol are usually more expensive than topical corticosteroids.
- Retinoids. Tazarotene (Tazorac, Avage) is available as a gel and cream and applied once or twice daily. The most common side effects are skin irritation and increased sensitivity to light.
- Tazarotene isn't recommended when you're pregnant or breast-feeding or if you intend to become pregnant.
- Calcineurin inhibitors. Calcineurin inhibitors — such as tacrolimus (Protopic) and pimecrolimus (Elidel) — reduce inflammation and plaque buildup. They can be especially helpful in areas of thin skin, such as around the eyes, where steroid creams or retinoids are too irritating or may cause harmful effects.
- Calcineurin inhibitors are not recommended when you're pregnant or breast-feeding or if you intend to become pregnant. This drug is also not intended for long-term use because of a potential increased risk of skin cancer and lymphoma.
- Salicylic acid. Salicylic acid shampoos and scalp solutions reduce the scaling of scalp psoriasis. It may be used alone, or to enhance the ability of other medications to more easily penetrate the skin.
- Coal tar. Coal tar reduces scaling, itching and inflammation. It's available over-the-counter or by prescription in various forms, such as shampoo, cream and oil. These products can irritate the skin. They're also messy, stain clothing and bedding, and can have a strong odor.
- Coal tar treatment isn't recommended for women who are pregnant or breast-feeding.
- Goeckerman therapy. Some doctors combine coal tar treatment with light therapy, which is known as Goeckerman therapy. The two therapies together are more effective than either alone because coal tar makes skin more receptive to UVB light.
- Anthralin. Anthralin (another tar product) is a cream used to slow skin cell growth. It can also remove scales and make skin smoother. It should not be used on the face or genitals. Anthralin can irritate skin, and it stains almost anything it touches. It's usually applied for a short time and then washed off.
Light therapy
Light therapy is a first-line treatment for moderate to severe psoriasis, either alone or in combination with medications. It involves exposing the skin to controlled amounts of natural or artificial light. Repeated treatments are necessary. Talk with your doctor about whether home phototherapy is an option for you.
- Sunlight. Brief, daily exposures to sunlight (heliotherapy) might improve psoriasis. Before beginning a sunlight regimen, ask your doctor about the safest way to use natural light for psoriasis treatment.
- UVB broadband. Controlled doses of UVB broadband light from an artificial light source can treat single patches, widespread psoriasis and psoriasis that doesn't improve with topical treatments. Short-term side effects might include redness, itching and dry skin. Moisturizing regularly can help ease your discomfort.
- UVB narrowband. UVB narrowband light therapy might be more effective than UVB broadband treatment and in many places has replaced broadband therapy. It's usually administered two or three times a week until the skin improves and then less frequently for maintenance therapy. Narrowband UVB phototherapy may cause more-severe and longer lasting burns, however.
- Psoralen plus ultraviolet A (PUVA). This treatment involves taking a light-sensitizing medication (psoralen) before exposure to UVA light. UVA light penetrates deeper into the skin than does UVB light, and psoralen makes the skin more responsive to UVA exposure.
- This more aggressive treatment consistently improves skin and is often used for more-severe cases of psoriasis. Short-term side effects include nausea, headache, burning and itching. Long-term side effects include dry and wrinkled skin, freckles, increased sun sensitivity, and increased risk of skin cancer, including melanoma.
- Excimer laser. With this form of light therapy, a strong UVB light targets only the affected skin. Excimer laser therapy requires fewer sessions than does traditional phototherapy because more powerful UVB light is used. Side effects can include redness and blistering.
Oral or injected medications
If you have moderate to severe psoriasis or other treatments haven't worked, your doctor may prescribe oral or injected (systemic) drugs. Because of the potential for severe side effects, some of these medications are used for only brief periods and might be alternated with other treatments.
- Steroids. If you have a few small, persistent psoriasis patches, your doctor might suggest an injection of triamcinolone right into the lesions.
- Retinoids. Acitretin (Soriatane) and other retinoids are pills used to reduce the production of skin cells. Side effects might include dry skin and muscle soreness. These drugs are not recommended when you're pregnant or breast-feeding or if you intend to become pregnant.
- Methotrexate. Usually administered weekly as a single oral dose, methotrexate (Trexall) decreases the production of skin cells and suppresses inflammation. It's less effective than adalimumab (Humira) and infliximab (Remicade). It might cause upset stomach, loss of appetite and fatigue. People taking methotrexate long term need ongoing testing to monitor their blood counts and liver function.
- Men and women should stop taking methotrexate at least three months before attempting to conceive. This drug is not recommended when you're breast-feeding.
- Cyclosporine. Taken orally for severe psoriasis, cyclosporine (Neoral) suppresses the immune system. It's similar to methotrexate in effectiveness but cannot be used continuously for more than a year. Like other immunosuppressant drugs, cyclosporine increases your risk of infection and other health problems, including cancer. People taking cyclosporine need ongoing monitoring of their blood pressure and kidney function.
- These drugs are not recommended when you're pregnant, breast-feeding or if you intend to become pregnant.
- Biologics. These drugs, usually administered by injection, alter the immune system in a way that disrupts the disease cycle and improves symptoms and signs of disease within weeks. Several of these drugs are approved for the treatment of moderate to severe psoriasis in people who haven't responded to first-line therapies. The therapeutic options are rapidly expanding. Examples include etanercept (Enbrel), infliximab (Remicade), adalimumab (Humira), ustekinumab (Stelara), secukinumab (Cosentyx) and ixekizumab (Taltz). These types of drugs are expensive and may or may not be covered by health insurance plans.
- Biologics must be used with caution because they carry the risk of suppressing your immune system in ways that increase your risk of serious infections. In particular, people taking these treatments must be screened for tuberculosis.
- Other medications. Thioguanine (Tabloid) and hydroxyurea (Droxia, Hydrea) are medications that can be used when other drugs can't be given. Apremilast (Otezla) is taken by mouth twice a day. It's especially effective at reducing itching. Talk with your doctor about possible side effects of these drugs.
Treatment considerations
Although doctors choose treatments based on the type and severity of psoriasis and the areas of skin affected, the traditional approach is to start with the mildest treatments — topical creams and ultraviolet light therapy (phototherapy) — in people with typical skin lesions (plaques) and then progress to stronger ones only if necessary. People with pustular or erythrodermic psoriasis or associated arthritis usually need systemic therapy from the beginning of treatment. The goal is to find the most effective way to slow cell turnover with the fewest possible side effects.
Alternative medicine
A number of alternative therapies claim to ease the symptoms of psoriasis, including special diets, creams, dietary supplements and herbs. None have definitively been proved effective. But some alternative therapies are deemed generally safe and might reduce itching and scaling in people with mild to moderate psoriasis. Other alternative therapies are useful in avoiding triggers, such as stress.
- Aloe extract cream. Taken from the leaves of the aloe vera plant, aloe extract cream may reduce redness, scaling, itching and inflammation. You might need to use the cream several times a day for a month or more to see any improvement in your skin.
- Fish oil supplements. Oral fish oil therapy used in combination with UVB therapy might reduce the amount of affected skin. Applying fish oil to the affected skin and covering it with a dressing for six hours a day for four weeks might improve scaling.
- Oregon grape. Also known as barberry, this product is applied to the skin and may reduce the severity of psoriasis.
- Essential oils. Essential oils used for aromatherapy have been shown to reduce stress and anxiety.
If you're considering dietary supplements or other alternative therapy to ease the symptoms of psoriasis, consult your doctor. He or she can help you weigh the pros and cons of specific alternative therapies.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
-
Graphites
30, 200 strength.
-
Nitric acid
30 strength.
-
Thuja occidentalis
30, 200 strength.
-
Mezereum
6, 30 strength.
-
Sulphur
30, 200 strength.
-
Tuberculinum
30, 200 strength.
-
Bacillinum
6, 30, 200 power.
-
Arsenicum iodatum
6, 30 strength.
-
Calcarea carbonica
30, 200 strength.
-
Ammonium carbonicum
30, 200 strength.
-
Acid chrysophanic
3X, 30X strength.
Disease yoga
Psoriasis and Learn More about Diseases

Brain tumor
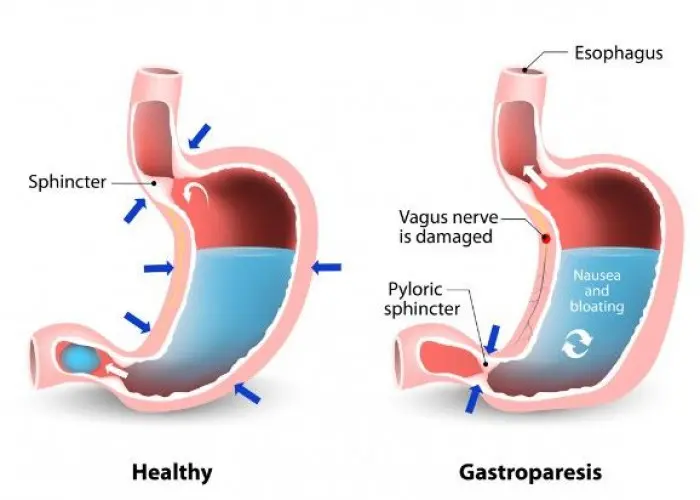
Gastroparesis

Tricuspid valve disease

Angelman syndrome

Pediatric thrombocytopenia
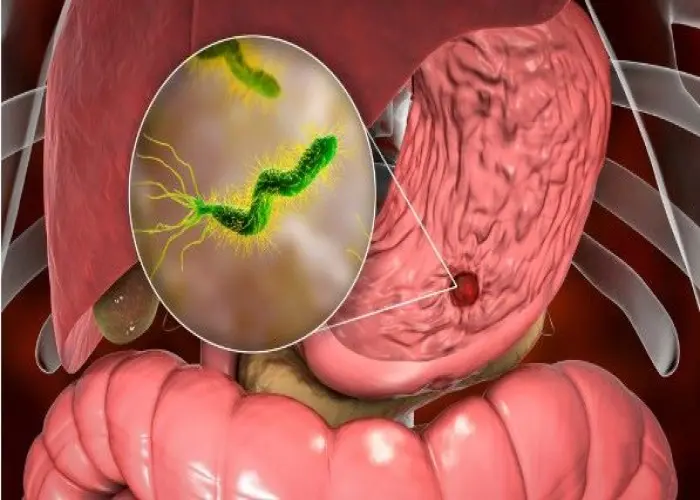
Duodenal Ulcer
Popliteal artery entrapment syndrome

Age spots (liver spots)
psoriasis, সোরিয়াসিস
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
