Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Pseudomembranous colitis
Pseudomembranous colitis is an inflammatory condition of the colon that is caused by an overgrowth of the bacterium Clostridium difficile (C. difficile). This overgrowth can be triggered by the use of antibiotics, which can disrupt the normal balance of bacteria in the gut and allow C. difficile to thrive.
The symptoms of pseudomembranous colitis can range from mild to severe and may include diarrhea, abdominal pain and cramping, fever, and dehydration. In severe cases, pseudomembranous colitis can lead to toxic megacolon, a potentially life-threatening condition characterized by severe inflammation and dilation of the colon.
Diagnosis of pseudomembranous colitis is typically done through a stool test that detects the presence of C. difficile toxins. In some cases, colonoscopy or sigmoidoscopy may be performed to examine the colon and take tissue samples for analysis.
Treatment for pseudomembranous colitis typically involves discontinuing the use of the offending antibiotic, if possible, and starting treatment with antibiotics that are effective against C. difficile, such as metronidazole or vancomycin. In severe cases, hospitalization and intravenous fluids and medications may be necessary.
Prevention of pseudomembranous colitis involves the judicious use of antibiotics, as well as hand hygiene and infection control measures to prevent the spread of C. difficile in healthcare settings. In some cases, probiotics or fecal microbiota transplantation may be used to restore the normal balance of bacteria in the gut and prevent recurrent infections.
Research Papers
Disease Signs and Symptoms
- Diarrhea
- Abdomen cramps
- Abdomen pain
- Fever
- Mucus with stool
- Nausea or vomiting
- Dehydration
Disease Causes
Pseudomembranous colitis
Your body usually keeps the many bacteria in your colon in a naturally healthy balance, but antibiotics and other medications can upset this balance. Pseudomembranous colitis occurs when certain bacteria — usually C. difficile — rapidly outgrow other bacteria that normally keep them in check. Certain toxins produced by C. difficile, which are usually present in only tiny amounts, rise to levels high enough to damage the colon.
While almost any antibiotic can cause pseudomembranous colitis, some antibiotics are more commonly linked to pseudomembranous colitis than others, including:
- Fluoroquinolones, such as ciprofloxacin (Cipro) and levofloxacin
- Penicillins, such as amoxicillin and ampicillin
- Clindamycin (Cleocin)
- Cephalosporins, such as cefixime (Suprax)
Other causes
Other medications besides antibiotics can sometimes cause pseudomembranous colitis. Chemotherapy drugs that are used to treat cancer may disrupt the normal balance of bacteria in the colon.
Certain diseases that affect the colon, such as ulcerative colitis or Crohn's disease, may also predispose people to pseudomembranous colitis.
C. difficile spores are resistant to many common disinfectants and can be transmitted from the hands of health care professionals to patients. Increasingly, C. difficile has been reported in people with no known risk factors, including people with no recent health care contact or use of antibiotics. This is called community-acquired C. difficile.
Emergence of a new strain
An aggressive strain of C. difficile has emerged that produces far more toxins than other strains do. The new strain may be more resistant to certain medications and has shown up in people who haven't been in the hospital or taken antibiotics.
Disease Prevents
Pseudomembranous colitis
To help prevent the spread of C. difficile, hospitals and other health care facilities follow strict infection-control guidelines. If you have a friend or family member in a hospital or nursing home, don't be afraid to remind caregivers to follow the recommended precautions.
Preventive measures include:
- Hand-washing. Health care workers should practice good hand hygiene before and after treating each person in their care. In the event of a C. difficile outbreak, using soap and warm water is a better choice for hand hygiene, because alcohol-based hand sanitizers do not effectively destroy C. difficile spores. Visitors also should wash their hands with soap and warm water before and after leaving the room or using the bathroom.
- Contact precautions. People who are hospitalized with C. difficile have a private room or share a room with someone who has the same illness. Hospital staff and visitors wear disposable gloves and isolation gowns while in the room until at least 48 hours after diarrhea ends.
- Thorough cleaning. In any setting, all surfaces should be carefully disinfected with a product that contains chlorine bleach to destroy C. difficile spores.
- Avoid unnecessary use of antibiotics. Antibiotics are sometimes prescribed for viral illnesses that aren't helped by these drugs. Take a wait-and-see attitude with simple ailments. If you do need an antibiotic, ask your doctor to prescribe one that has a narrow range and that you take for the shortest time possible.
Disease Treatments
Treatment strategies include:
- Stopping the antibiotic or other medication that's thought to be causing your signs and symptoms, if possible. Sometimes, this may be enough to resolve your condition or at least ease signs, such as diarrhea.
- Starting an antibiotic likely to be effective against C. difficile. If you still experience signs and symptoms, your doctor may use a different antibiotic to treat C. difficile. This allows the normal bacteria to grow back, restoring the healthy balance of bacteria in your colon.
- You may be given antibiotics by mouth, through a vein or through a tube inserted through the nose into the stomach (nasogastric tube). Depending on your condition, vancomycin or fidaxomicin (Dificid) is most often used. If these drugs are not available or cannot be tolerated, then metronidazole (Flagyl) may be used.
- For severe disease, your doctor may prescribe vancomycin by mouth combined with intravenous metronidazole or a vancomycin enema.
- Having fecal microbial transplantation (FMT). If your condition is extremely severe or you have had more than one recurrence of the infection, you may be given a transplant of stool (fecal transplant) from a healthy donor to restore the balance of bacteria in your colon. The donor stool may be delivered through a nasogastric tube, inserted into the colon or placed in a capsule you swallow. Doctors may use a combination of antibiotic treatment followed by FMT.
Once you begin treatment for pseudomembranous colitis, signs and symptoms may begin to improve within a few days.
Treating recurring pseudomembranous colitis
The natural occurrence of new, more-aggressive strains of C. difficile, which are more resistant to antibiotics, has made treating pseudomembranous colitis increasingly difficult and recurrences more common. With each recurrence, your chance of having an additional recurrence increases.
Treatment options may include:
- Repeat antibiotics. You may need a second or third round of antibiotics to resolve your condition and may need a longer duration of therapy.
- Surgery. Surgery may be an option in people who have progressive organ failure, rupture of the colon and inflammation of the lining of the abdominal wall (peritonitis). Surgery has typically involved removing all or part of the colon (total or subtotal colectomy).
- A newer surgery that involves laparoscopically creating a loop of colon and cleaning it (loop ileostomy and colonic lavage) is less invasive and has had positive results.
- Fecal microbial transplantation (FMT). FMT is used to treat recurrent pseudomembranous colitis. You'll receive healthy, cleaned stool in a capsule, nasogastrically or inserted into your colon.
- Bezlotoxumab (Zinplava). The U.S. Food and Drug Administration (FDA) has approved the use of human monoclonal antibody bezlotoxumab to reduce the risk of recurrence of C. difficile infection. Used in combination with antibiotics, bezlotoxumab has been shown to significantly reduce the recurrence of infection. However, cost may be a limiting factor.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Pseudomembranous colitis and Learn More about Diseases

N/A
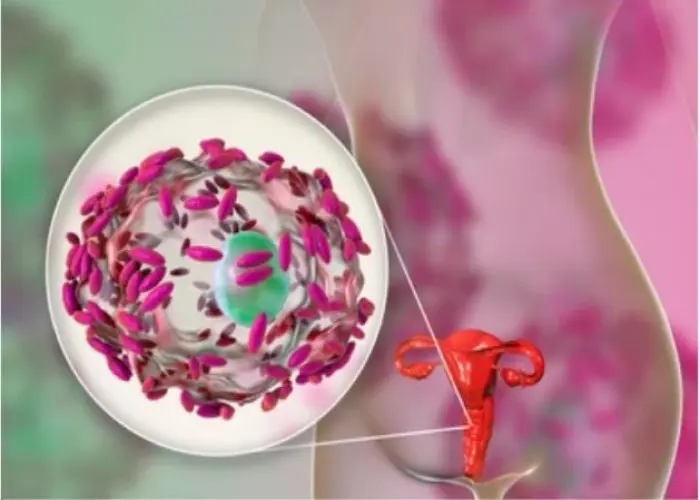
Bacterial vaginosis

Rheumatic fever

Encopresis

Vocal cord paralysis
Epilepsy
Cervical cancer

Premature birth
pseudomembranous colitis, সিওডুমেমব্রেনাস কোলাইটিস
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.