 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Posterior vaginal prolapse (Rectocele)

A posterior vaginal prolapse, also known as a rectocele, occurs when the tissue between the rectum and the vagina weakens and allows the rectum to push into or protrude into the vagina. This can happen when the muscles and tissues in the pelvic floor become weakened due to aging, childbirth, or other factors.
Symptoms of a posterior vaginal prolapse may include a feeling of pressure or fullness in the vagina or rectum, a sensation of a bulge or lump in the vagina, difficulty with bowel movements, and discomfort or pain during sexual intercourse.
Diagnosis of a posterior vaginal prolapse may involve a pelvic exam to visualize the prolapse and evaluate its severity. Additional tests, such as a defecography or magnetic resonance imaging (MRI), may be ordered to evaluate the extent of the prolapse and any associated structural abnormalities.
Treatment options for a posterior vaginal prolapse may include pelvic floor exercises to strengthen the muscles that support the pelvic organs, using a pessary to provide additional support to the vaginal wall, or surgical repair to restore the normal position of the pelvic organs. The choice of treatment will depend on the severity of the prolapse and the individual's overall health and preferences.
It is important to seek medical attention if symptoms of a posterior vaginal prolapse are present, as this condition can lead to significant discomfort and affect quality of life. Early diagnosis and treatment can help prevent complications and improve outcomes.
Research Papers
Disease Signs and Symptoms
- Frequent bowel movements
- Fullness in abdomen
- Difficulty having a bowel movement
- Pain that lasts three months or longer after the shingles rash has healed.
- The associated pain has been described as burning, sharp and jabbing, or deep and aching.
- People with the condition often can't bear even the touch of clothing on the affected skin (allodynia).
Disease Causes
Posterior vaginal prolapse (rectocele)
Posterior vaginal prolapse results from pressure on the pelvic floor. Causes of increased pelvic floor pressure include:
- Chronic constipation or straining with bowel movements
- Chronic cough or bronchitis
- Repeated heavy lifting
- Being overweight or obese
Pregnancy and childbirth
The muscles, ligaments and connective tissue that support your vagina become stretched and weakened during pregnancy, labor and delivery. The more pregnancies you have, the greater your chance of developing posterior vaginal prolapse.
Women who have had only cesarean deliveries are less likely to develop posterior vaginal prolapse, but still may.
Disease Prevents
Posterior vaginal prolapse (rectocele)
To reduce your risk of worsening posterior vaginal prolapse, try to:
- Perform Kegel exercises regularly. These exercises can strengthen your pelvic floor muscles — especially important after you have a baby.
- Treat and prevent constipation. Drink plenty of fluids and eat high-fiber foods, such as fruits, vegetables, beans and whole-grain cereals.
- Avoid heavy lifting and lift correctly. When lifting, use your legs instead of your waist or back.
- Control coughing. Get treatment for a chronic cough or bronchitis, and don't smoke.
- Avoid weight gain. Talk with your doctor to determine your ideal weight and get advice on weight-loss strategies, if you need them.
Disease Treatments
Treatment depends on the severity of the posterior vaginal prolapse. Your doctor might recommend:
- Observation. If your posterior vaginal prolapse causes few or no symptoms, simple self-care measures — such as performing Kegel exercises to strengthen your pelvic muscles — may provide relief.
- Pessary. A vaginal pessary is a plastic or rubber ring inserted into your vagina to support the bulging tissues. A pessary must be removed regularly for cleaning.
Surgery
Surgical repair might be needed if:
- The posterior vaginal prolapse protrudes outside your vagina and is especially bothersome.
- You have prolapse of other pelvic organs in addition to posterior vaginal prolapse that is bothersome. Surgical repair for each condition can be completed at the same time.
The surgery usually consists of removing excess, stretched tissue that forms the vaginal bulge and placing stitches (sutures) to support pelvic structures. A mesh patch might be inserted to support and strengthen the fascia.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Posterior vaginal prolapse (Rectocele) and Learn More about Diseases
Zollinger-Ellison syndrome

Migraine with aura
Common variable immunodeficiency
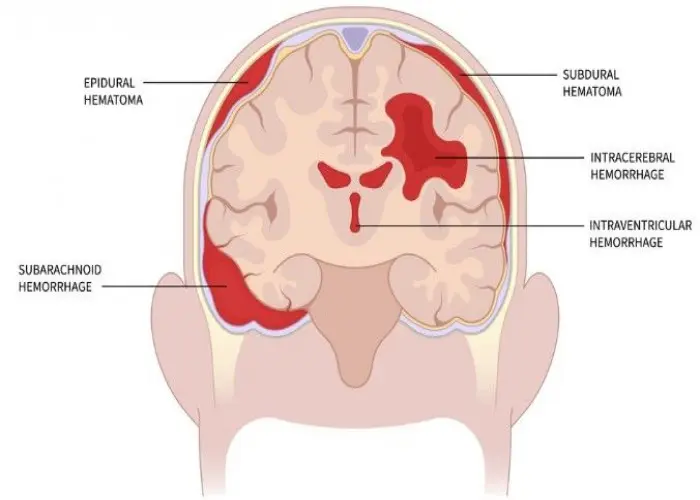
Intracranial hematoma
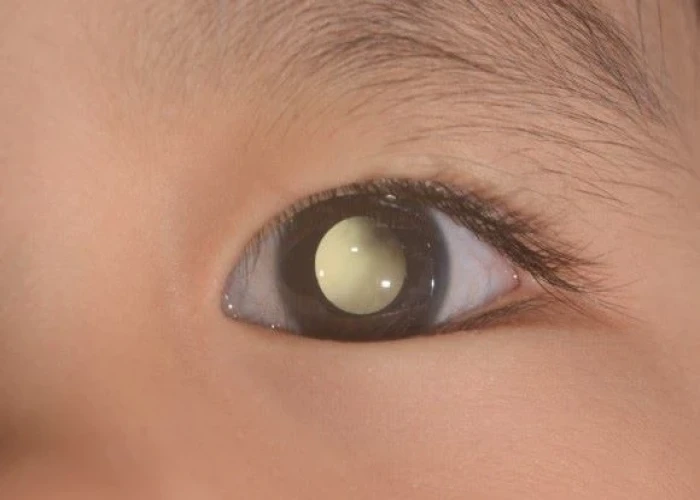
Retinoblastoma

Burning mouth syndrome

Pinched nerve
Myelofibrosis
posterior vaginal prolapse, rectocele, পোস্টেরিয়র ভ্যাজাইনাল প্রোল্যাপস, কোষীয় যোনি প্রলাপস, রেক্টোসিল
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
