 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Overactive bladder
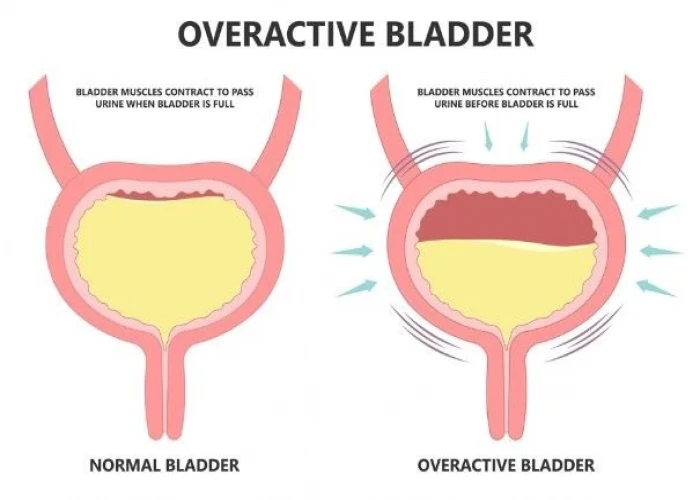
Overactive bladder (OAB) is a condition in which the bladder muscles contract involuntarily and cause the urge to urinate frequently, sometimes even without warning. This condition can cause discomfort, embarrassment, and interfere with daily activities.
Symptoms of OAB include:
- Urgency to urinate that cannot be postponed
- Frequent urination (usually more than eight times per day)
- Urinary incontinence (leakage of urine)
Some people with OAB may also experience nocturia, which is the need to urinate at night.
The exact cause of OAB is unknown, but it is believed to be related to problems with nerve signals between the bladder and the brain. Certain factors can also contribute to OAB, such as urinary tract infections, bladder stones, and bladder cancer.
Treatment of OAB may involve behavioral modifications, such as bladder training exercises and pelvic muscle exercises, as well as medications to relax the bladder muscles or reduce the frequency of contractions. In some cases, nerve stimulation or surgery may be necessary.
Prevention of OAB involves maintaining good bladder health, such as drinking enough water, avoiding caffeine and alcohol, and practicing good hygiene to prevent urinary tract infections. It is also important to manage any underlying conditions that can contribute to OAB, such as diabetes or prostate problems.
Research Papers
Disease Signs and Symptoms
- Frequent urination
- Wake up more than two times in the night to urinate (nocturia)
- Urinate frequently, usually eight or more times in 24 hours
Disease Causes
Overactive bladder
Normal bladder function
The kidneys produce urine, which drains into your bladder. When you urinate, urine passes from your bladder through a tube called the urethra (u-REE-thruh). A muscle in the urethra called the sphincter opens to release urine out of the body.
In women, the urethral opening is located just above the vaginal opening. In men, the urethral opening is at the tip of the penis.
As your bladder fills, nerve signals sent to your brain eventually trigger the need to urinate. When you urinate, these nerve signals coordinate the relaxation of the pelvic floor muscles and the muscles of the urethra (urinary sphincter muscles). The muscles of the bladder tighten (contract), pushing the urine out.
Involuntary bladder contractions
Overactive bladder occurs because the muscles of the bladder start to contract involuntarily even when the volume of urine in your bladder is low. These involuntary contractions create an urgent need to urinate.
Several conditions may contribute to signs and symptoms of overactive bladder, including:
- Neurological disorders, such as stroke and multiple sclerosis
- Diabetes
- Urinary tract infections that can cause symptoms similar to those of an overactive bladder
- Hormonal changes during menopause in women
- Abnormalities in the bladder, such as tumors or bladder stones
- Factors that obstruct bladder outflow — enlarged prostate, constipation or previous operations to treat other forms of incontinence
Other factors that may be associated with your symptoms include:
- Medications that cause a rapid increase in urine production or require that you take them with lots of fluids
- Excess consumption of caffeine or alcohol
- Declining cognitive function due to aging, which may make it more difficult for your bladder to understand the signals it receives from your brain
- Difficulty walking, which can lead to bladder urgency if you're unable to get to the bathroom quickly
- Incomplete bladder emptying, which may lead to symptoms of overactive bladder, as you have little urine storage space left
The specific cause of an overactive bladder may be unknown.
Disease Prevents
Overactive bladder
These healthy lifestyle choices may reduce your risk of overactive bladder:
- Maintain a healthy weight.
- Get regular, daily physical activity and exercise.
- Limit consumption of caffeine and alcohol.
- Quit smoking.
- Manage chronic conditions, such as diabetes, that might contribute to overactive bladder symptoms.
- Learn where your pelvic floor muscles are and then strengthen them by doing Kegel exercises — tighten (contract) the muscles, hold the contraction for two seconds and relax the muscles for three seconds. Work up to holding the contraction for five seconds and then 10 seconds at a time. Do three sets of 10 repetitions each day.
Disease Treatments
A combination of treatment strategies may be the best approach to relieve overactive bladder symptoms.
Behavioral therapies
Behavioral interventions are the first choice in helping manage an overactive bladder. They're often effective, and they carry no side effects. Behavioral interventions may include:
- Pelvic floor muscle exercises. Kegel exercises strengthen your pelvic floor muscles and urinary sphincter. These strengthened muscles can help you stop the bladder's involuntary contractions.
- Your doctor or a physical therapist can help you learn how to do Kegel exercises correctly. Just like any other exercise routine, how well Kegel exercises work for you depends on whether you perform them regularly.
- Biofeedback. During biofeedback, you're connected to electrical sensors that help you measure and receive information about your body. The biofeedback sensors teach you how to make subtle changes in your body, such as strengthening your pelvic muscles so that when you have feelings of urgency you're better able to suppress them.
- Healthy weight. If you're overweight, losing weight may ease symptoms. Weight loss may help if you also have stress urinary incontinence.
- Scheduled toilet trips. Setting a schedule for toileting — for example, every two to four hours — gets you on track to urinate at the same times every day rather than waiting until you feel the urge to urinate.
- Intermittent catheterization. If you are not able to empty your bladder well, using a catheter periodically to empty your bladder completely helps your bladder do what it can't do by itself. Ask your doctor if this approach is right for you.
- Absorbent pads. Wearing absorbent pads or undergarments can protect your clothing and help you avoid embarrassing incidents, which means that you won't have to limit your activities. Absorbent garments come in a variety of sizes and absorbency levels.
- Bladder training. Bladder training involves training yourself to delay voiding when you feel an urge to urinate. You begin with small delays, such as 30 minutes, and gradually work your way up to urinating every three to four hours. Bladder training is possible only if you're able to tighten (contract) your pelvic floor muscles successfully.
Medications
After menopause, vaginal estrogen therapy can help strengthen the muscles and tissues in the urethra and vaginal area. Vaginal estrogen comes in the form of cream, suppository, tablet, or ring, and can significantly improve symptoms of overactive bladder.
Medications that relax the bladder can be helpful for relieving symptoms of overactive bladder and reducing episodes of urge incontinence. These drugs include:
- Tolterodine (Detrol)
- Oxybutynin, which can be taken as a pill (Ditropan XL) or used as a skin patch (Oxytrol) or gel (Gelnique)
- Trospium
- Solifenacin (Vesicare)
- Darifenacin (Enablex)
- Fesoterodine (Toviaz)
- Mirabegron (Myrbetriq)
Common side effects of most of these drugs include dry eyes and dry mouth, but drinking water to quench thirst can aggravate symptoms of overactive bladder. Constipation — another potential side effect — can aggravate your bladder symptoms. Extended-release forms of these medications, including the skin patch or gel, may cause fewer side effects.
Your doctor may recommend that you sip small amounts of water or suck on a piece of sugar-free candy or chew sugar-free gum to relieve dry mouth, and use eyedrops to keep your eyes moist. Over-the-counter preparations, such as Biotene products, can be helpful for long-term dry mouth. To avoid constipation, your doctor might recommend a fiber-rich diet or use of stool softeners.
Bladder injections
OnabotulinumtoxinA (ON-ah-boch-yoo-lih-num-tox-in-A), also called Botox, is a protein from the bacteria that cause botulism illness. Used in small doses directly injected into bladder tissues, this protein relaxes the muscles.
Studies show that it may be useful for severe urge incontinence. The temporary effects generally last six months or more, but repeat injections are necessary.
Side effects from these injections include urinary tract infections and urinary retention. If you're considering Botox treatments, you should be willing and able to catheterize yourself if urinary retention occurs.
Nerve stimulation
Regulating the nerve impulses to your bladder can improve overactive bladder symptoms.
One procedure uses a thin wire placed close to the sacral nerves — which carry signals to your bladder — where they pass near your tailbone.
This minimally invasive procedure is often done with a trial of a temporary wire implanted under the skin in your lower back. Sometimes it may be done as an advanced procedure in which the permanent electrode is implanted and a longer trial is performed. Your doctor then uses a hand-held device connected to the wire to deliver electrical impulses to your bladder, similar to what a pacemaker does for the heart. If it helps with your symptoms, a permanent, battery-powered pulse generator is surgically implanted to help regulate the nerve rhythm.
Percutaneous tibial nerve stimulation (PTNS)
This procedure uses a thin needle that is placed through the skin near your ankle to send electrical stimulation from a nerve in your leg (tibial nerve) to your spine, where it connects with the nerves that control the bladder.
PTNS treatments are delivered once a week for 12 weeks to help treat symptoms of overactive bladder. You will likely need maintenance treatments every three to four weeks to keep symptoms under control.
Surgery
Surgery to treat overactive bladder is reserved for people with severe symptoms who don't respond to other treatments. The goal is to improve the bladder's ability to store urine and reduce pressure in the bladder. However, these procedures won't help relieve bladder pain. These procedures include:
- Surgery to increase bladder capacity. This procedure uses pieces of your bowel to replace a portion of your bladder. This surgery is used only in cases of severe urge incontinence that doesn't respond to any other, more-conservative treatment measures. If you have this surgery, you may need to use a catheter intermittently for the rest of your life to empty your bladder.
- Bladder removal. This procedure is used as a last resort and involves removing the bladder and surgically constructing a replacement bladder (neobladder) or an opening in the body (stoma) to attach a bag on the skin to collect urine.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Overactive bladder and Learn More about Diseases

Bell's palsy
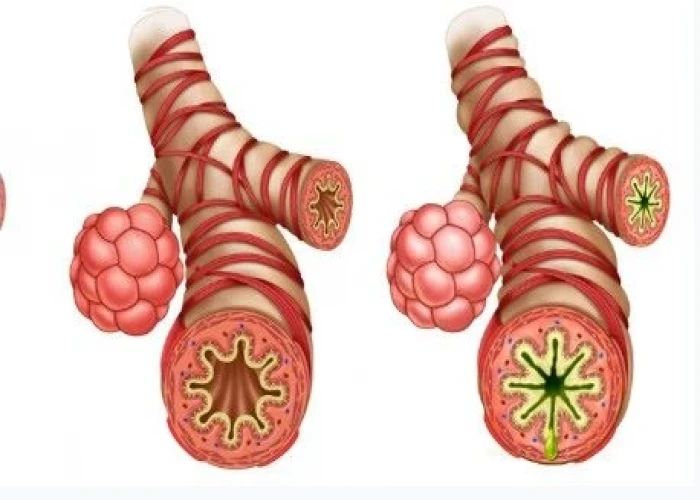
Occupational asthma

Yeast infection (vaginal)
Neuroendocrine tumors
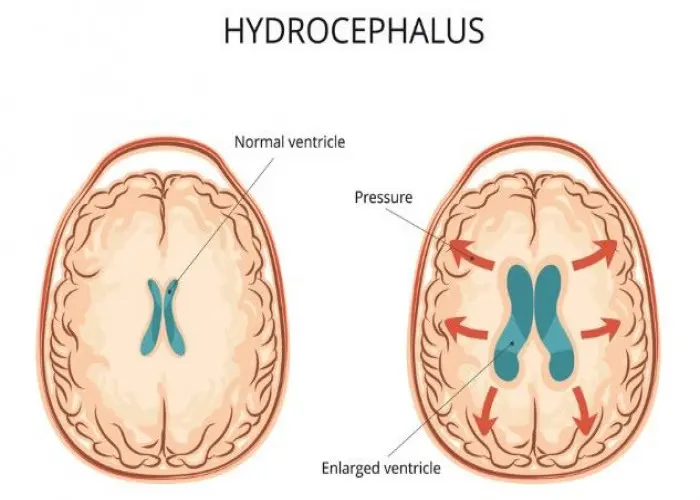
Hydrocephalus
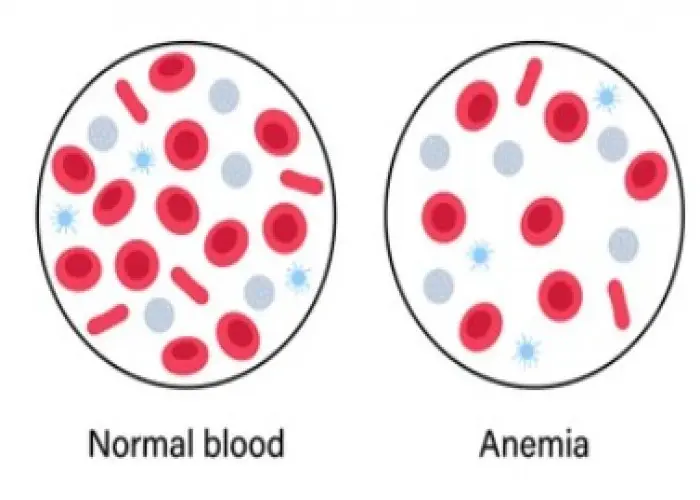
Anemia

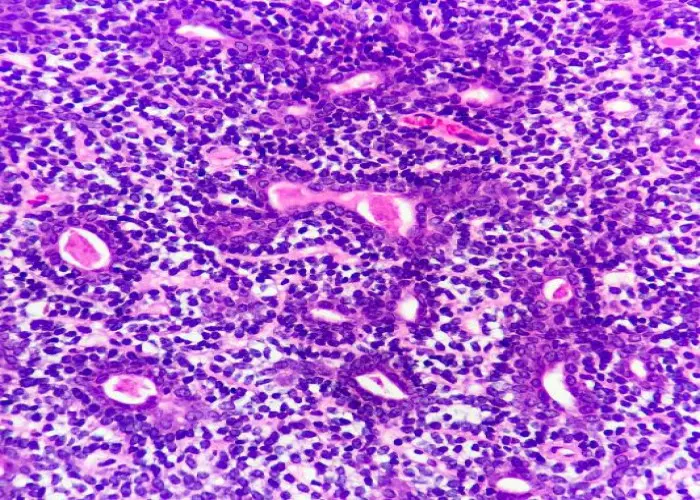
Desmoplastic small round cell tumors
Adnexal tumors
overactive bladder, ওভারভেটিভ ব্লাডার
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
