 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Persistent depressive disorder (dysthymia)

Persistent depressive disorder (PDD), also known as dysthymia, is a chronic form of depression that is characterized by low mood and feelings of sadness, hopelessness, and worthlessness that last for at least two years or longer. While the symptoms of PDD are generally less severe than those of major depression, they are more persistent and can have a significant impact on a person's quality of life.
Symptoms of PDD may include:
- Persistent feelings of sadness or emptiness
- Loss of interest or pleasure in activities that were once enjoyable
- Fatigue or low energy
- Difficulty sleeping or oversleeping
- Changes in appetite or weight
- Difficulty concentrating or making decisions
- Feelings of hopelessness or worthlessness
- Thoughts of suicide or self-harm
The exact cause of PDD is not known, but it is believed to be related to a combination of genetic, environmental, and psychological factors. Risk factors for PDD may include a family history of depression, chronic stress or trauma, and low levels of social support.
Diagnosis of PDD may involve a physical exam, a psychological evaluation, and screening for other medical conditions that may be contributing to the symptoms. Treatment may include a combination of psychotherapy, medication, and lifestyle changes, such as regular exercise, a healthy diet, and stress management techniques. Cognitive behavioral therapy (CBT) and interpersonal therapy (IPT) have been found to be effective treatments for PDD.
The prognosis for PDD varies depending on the severity of the symptoms, the individual's response to treatment, and the presence of any co-occurring medical or psychological conditions. With appropriate treatment, many people with PDD can achieve significant symptom relief and improve their overall quality of life.
Research Papers
Disease Signs and Symptoms
- Loss of interest in daily activities
- Decreased activity, effectiveness and productivity
- Trouble concentrating and trouble to make decisions
- Low self-esteem, self-criticism or feeling incapable
- Loss of appetite
- Irritability
- Difficulty concentrating
- Decreased energy
- Hopeless
- Feelings of sadness, tearfulness, emptiness or hopelessness
- Feelings of guilt and worries over the past
Disease Causes
Persistent depressive disorder (dysthymia)
The exact cause of persistent depressive disorder isn't known. As with major depression, it may involve more than one cause, such as:
- Biological differences. People with persistent depressive disorder may have physical changes in their brains. The significance of these changes is still uncertain, but they may eventually help pinpoint causes.
- Brain chemistry. Neurotransmitters are naturally occurring brain chemicals that likely play a role in depression. Recent research indicates that changes in the function and effect of these neurotransmitters and how they interact with neurocircuits involved in maintaining mood stability may play a significant role in depression and its treatment.
- Inherited traits. Persistent depressive disorder appears to be more common in people whose blood relatives also have the condition. Researchers are trying to find genes that may be involved in causing depression.
- Life events. As with major depression, traumatic events such as the loss of a loved one, financial problems or a high level of stress can trigger persistent depressive disorder in some people
Disease Prevents
Persistent depressive disorder (dysthymia)
There's no sure way to prevent persistent depressive disorder. Because it often starts in childhood or during the teenage years, identifying children at risk of the condition may help them get early treatment.
Strategies that may help ward off symptoms include the following:
- Take steps to control stress, to increase your resilience and to boost your self-esteem.
- Reach out to family and friends, especially in times of crisis, to help you weather rough spells.
- Get treatment at the earliest sign of a problem to help prevent symptoms from worsening.
- Consider getting long-term maintenance treatment to help prevent a relapse of symptoms.
Disease Treatments
The two main treatments for persistent depressive disorder are medications and talk therapy (psychotherapy). The treatment approach your doctor recommends depends on factors such as:
- Severity of your symptoms
- Your desire to address emotional or situational issues affecting your life
- Your personal preferences
- Previous treatment methods
- Your ability to tolerate medications
- Other emotional problems you may have
Psychotherapy may be the first recommendation for children and adolescents with persistent depressive disorder, but that depends on the individual. Sometimes antidepressants are also needed.
Medications
The types of antidepressants most commonly used to treat persistent depressive disorder include:
- Selective serotonin reuptake inhibitors (SSRIs)
- Tricyclic antidepressants (TCAs)
- Serotonin and norepinephrine reuptake inhibitors (SNRIs)
Talk with your doctor or pharmacist about possible side effects.
Finding the right medication
You may need to try several medications or a combination before you find one that works. This requires patience, as some medications take several weeks or longer for full effect and for side effects to ease as your body adjusts.
Don't stop taking an antidepressant without talking to your doctor — your doctor can help you gradually and safely decrease your dose. Stopping treatment abruptly or missing several doses may cause withdrawal-like symptoms, and quitting suddenly may cause a sudden worsening of depression.
When you have persistent depressive disorder, you may need to take antidepressants long term to keep symptoms under control
Antidepressants and pregnancy
If you're pregnant or breast-feeding, some antidepressants may pose an increased health risk to your unborn baby or nursing child. Talk to your doctor if you become pregnant or are planning on becoming pregnant.
FDA alert on antidepressants
Although antidepressants are generally safe when taken as directed, the FDA requires all antidepressants to carry a black box warning, the strictest warning for prescriptions. In some cases, children, teens and young adults under 25 may have an increase in suicidal thoughts or behavior when taking antidepressants, especially in the first few weeks after starting or when the dose is changed.
Anyone taking an antidepressant should be watched closely for worsening depression or unusual behavior, especially when first beginning a new medication or with a change in dosage. If your teen has suicidal thoughts while taking an antidepressant, immediately contact your doctor or get emergency help.
Keep in mind that antidepressants are more likely to reduce suicide risk in the long run by improving mood.
Psychotherapy
Psychotherapy is a general term for treating depression by talking about your condition and related issues with a mental health professional. Psychotherapy is also known as talk therapy or psychological counseling.
Different types of psychotherapy, such as cognitive behavioral therapy, can be effective for persistent depressive disorder. You and your therapist can discuss which type of therapy is right for you, your goals for therapy and other issues, such as the length of treatment.
Psychotherapy can help you:
- Adjust to a crisis or other current difficulty
- Identify issues that contribute to your depression and change behaviors that make it worse
- Identify negative beliefs and behaviors and replace them with healthy, positive ones
- Find better ways to cope and solve problems
- Explore relationships and experiences, and develop positive interactions with others
- Regain a sense of satisfaction and control in your life and help ease depression symptoms, such as hopelessness and anger
- Learn to set realistic goals for your life
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Persistent depressive disorder (dysthymia) and Learn More about Diseases

Klinefelter syndrome

Non-Hodgkin's lymphoma

Yellow fever

Celiac disease

Bladder exstrophy

Medication overuse headaches
Dizziness
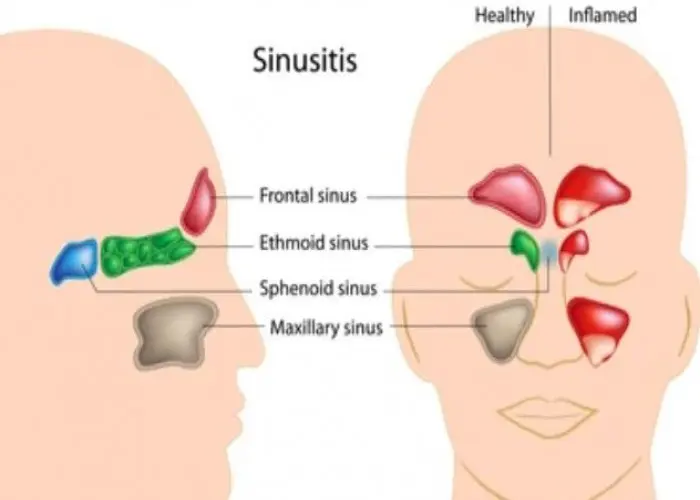
Chronic sinusitis
Persistent depressive disorder, dysthymia, ক্রমাগত ডিপ্রেশন ডিসঅর্ডার, ডিসস্টাইমিয়া
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
