Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Myelofibrosis
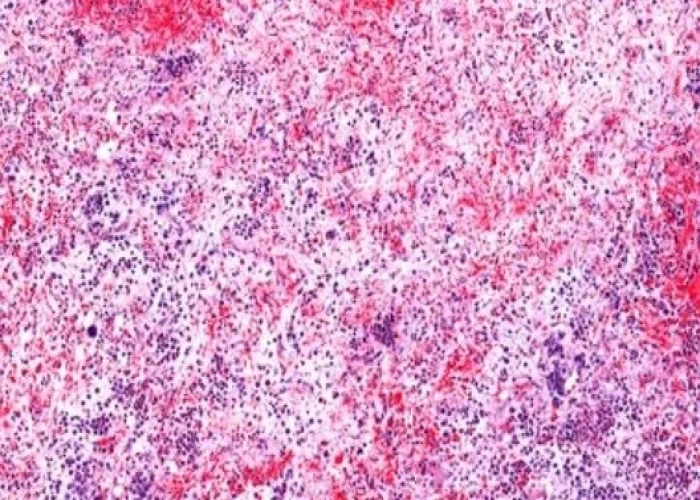
Myelofibrosis is a type of chronic leukemia that affects the bone marrow, which is the spongy tissue inside the bones that produces blood cells. It is characterized by the abnormal growth of fibrous tissue within the bone marrow, which can lead to a decrease in the production of blood cells.
The cause of myelofibrosis is not fully understood, but it is believed to be related to mutations in certain genes that control the growth and differentiation of blood cells. Some risk factors for developing myelofibrosis include exposure to certain chemicals, radiation exposure, and a family history of the disease.
Symptoms of myelofibrosis may include fatigue, weakness, shortness of breath, bruising, bleeding, and an enlarged spleen. Treatment options for myelofibrosis depend on the stage of the disease and may include medications to manage symptoms, blood transfusions, chemotherapy, stem cell transplantation, and targeted therapies that target the genetic mutations associated with the disease.
Research Papers
Disease Signs and Symptoms
- Excessive sweat
- Night sweats
- Fever
- Bone pain
- Pain or fullness below ribs on the left side, due to an enlarged spleen
Disease Causes
Myelofibrosis
Myelofibrosis occurs when bone marrow stem cells develop changes (mutations) in their DNA. The stem cells have the ability to replicate and divide into the multiple specialized cells that make up your blood — red blood cells, white blood cells and platelets.
It's not clear what causes the genetic mutations in bone marrow stem cells.
As the mutated blood stem cells replicate and divide, they pass along the mutations to the new cells. As more and more of these mutated cells are created, they begin to have serious effects on blood production.
The end result is usually a lack of red blood cells — which causes the anemia characteristic of myelofibrosis — and an overabundance of white blood cells and varying levels of platelets. In people with myelofibrosis, the normally spongy bone marrow becomes scarred.
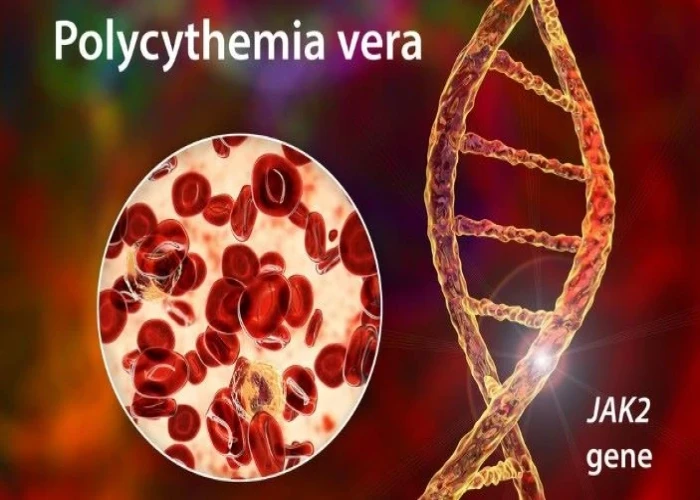
Several specific gene mutations have been identified in people with myelofibrosis. The most common is the Janus kinase 2 (JAK2) gene mutation. Other less common mutations include CALR and MPL. Some people with myelofibrosis don't have any identifiable gene mutations. Knowing whether these gene mutations are associated with your myelofibrosis helps determine your prognosis and your treatment.
Disease Prevents
Disease Treatments
The goal of treatment for most people with myelofibrosis is to provide relief from signs and symptoms of the disease. For some, a bone marrow transplant may provide a chance for a cure, but this treatment is very hard on the body and it might not be an option for many people.
In order to determine which myelofibrosis treatments are most likely to benefit you, your doctor may use one or more formulas to assess your condition. These formulas take into account many aspects of your cancer and your overall health to assign a risk category that indicates the aggressiveness of the disease.
Low-risk myelofibrosis may not require immediate treatment, while people with high-risk myelofibrosis may consider an aggressive treatment, such as bone marrow transplant. For intermediate-risk myelofibrosis, treatment is usually directed at managing symptoms.
Immediate treatment may not be necessary
Myelofibrosis treatment may not be necessary if you aren't experiencing symptoms. You might not need treatment right away if you don't have an enlarged spleen and you don't have anemia or your anemia is very mild. Rather than treatment, your doctor is likely to monitor your health closely through regular checkups and exams, watching for any signs of disease progression. Some people remain symptom-free for years.
Treatments for anemia
If myelofibrosis is causing severe anemia, you may consider treatment, such as:
- Blood transfusions. If you have severe anemia, periodic blood transfusions can increase your red blood cell count and ease anemia symptoms, such as fatigue and weakness. Sometimes, medications can help improve anemia.
- Androgen therapy. Taking a synthetic version of the male hormone androgen may promote red blood cell production and may improve severe anemia in some people. Androgen therapy does have risks, including liver damage and masculinizing effects in women.
- Thalidomide and related medications. Thalidomide (Thalomid) and the related drug lenalidomide (Revlimid) may help improve blood cell counts and may also relieve an enlarged spleen. These drugs may be combined with steroid medications. Thalidomide and related drugs carry a risk of serious birth defects and require special precautions.
Treatments for an enlarged spleen
If an enlarged spleen is causing complications, your doctor may recommend treatment. Your options may include:
- Targeted drug therapy. Targeted drug treatments focus on specific abnormalities present within cancer cells. Targeted treatments for myelofibrosis focus on cells with the JAK2 gene mutation. These treatments are used to reduce symptoms of an enlarged spleen.
- Chemotherapy. Chemotherapy uses powerful drugs to kill cancer cells. Chemotherapy drugs may reduce the size of an enlarged spleen and relieve related symptoms, such as pain.
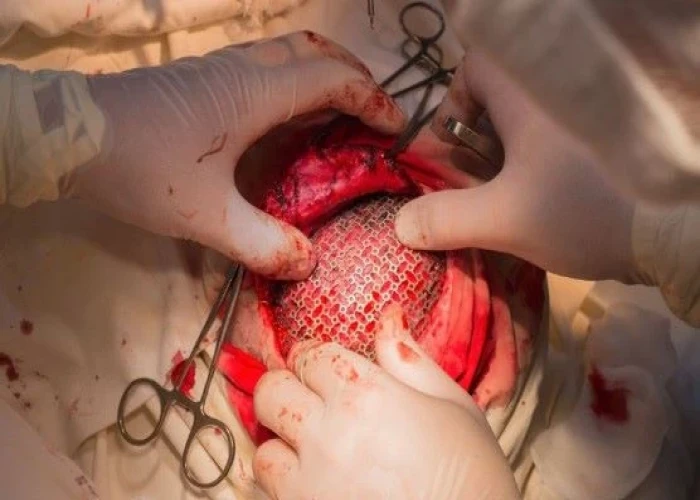
- Surgical removal of the spleen (splenectomy). If your spleen becomes so large that it causes you pain and begins to cause harmful complications — and if you don't respond to other forms of therapy — you may benefit from having your spleen surgically removed.
- Risks include infection, excessive bleeding and blood clot formation leading to stroke or pulmonary embolism. After the procedure, some people experience liver enlargement and an abnormal increase in platelet count.
- Radiation therapy. Radiation uses high-powered beams, such as X-rays and protons, to kill cancer cells. Radiation therapy can help reduce the size of the spleen when surgical removal isn't an option.
Bone marrow transplant
A bone marrow transplant, also called a stem cell transplant, is a procedure to replace your diseased bone marrow using healthy blood stem cells. For myelofibrosis, the procedure uses stem cells from a donor (allogeneic stem cell transplant).
This treatment has the potential to cure myelofibrosis, but it also carries a high risk of life-threatening side effects, including a risk that the new stem cells will react against your body's healthy tissues (graft-versus-host disease).
Many people with myelofibrosis, because of age, stability of the disease or other health problems, don't qualify for this treatment.
Prior to a bone marrow transplant, you receive chemotherapy or radiation therapy to destroy your diseased bone marrow. Then you receive infusions of stem cells from a compatible donor.
Supportive (palliative) care
Palliative care is specialized medical care that focuses on providing relief from pain and other symptoms of a serious illness. Palliative care specialists work with you, your family and your other doctors to provide an extra layer of support that complements your ongoing care. Palliative care can be used while undergoing other aggressive treatments, such as surgery, chemotherapy or radiation therapy.
When palliative care is used along with all of the other appropriate treatments, people with cancer may feel better and live longer.
Palliative care is provided by a team of doctors, nurses and other specially trained professionals. Palliative care teams aim to improve the quality of life for people with cancer and their families. This form of care is offered alongside curative or other treatments you may be receiving.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Myelofibrosis and Learn More about Diseases

Cardiogenic shock

Ruptured spleen
Polycythemia vera

Broken ribs

Hypoplastic left heart syndrome
Pediatric brain tumors

Body lice

Seborrheic keratosis
myelofibrosis, মাইলোফাইব্রোসিস
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.