Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
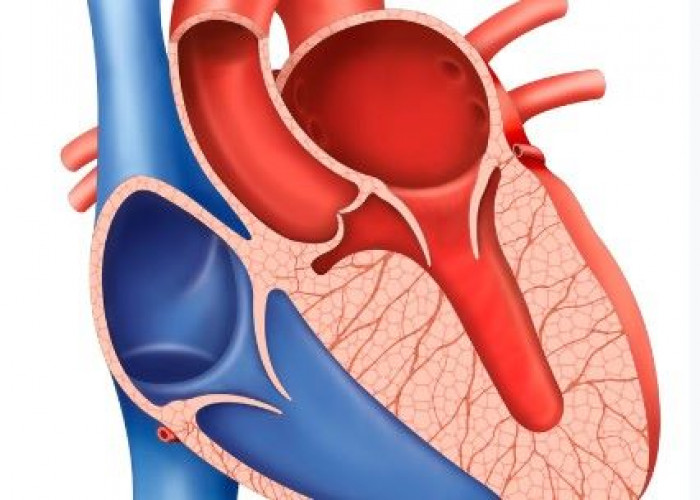
Hypertrophic cardiomyopathy
Hypertrophic cardiomyopathy (HCM) is a genetic cardiovascular disorder characterized by abnormal thickening of the heart muscle, which can make it difficult for the heart to pump blood efficiently. HCM is a common cause of sudden cardiac death in young people and athletes.
HCM can be caused by mutations in genes that affect the structure of the heart muscle cells. In many cases, HCM is inherited from a parent who has the condition, although some people may develop the disorder due to a spontaneous mutation.
Symptoms of HCM can vary but may include shortness of breath, chest pain, fainting, dizziness, and palpitations. Some people with HCM may not experience any symptoms.
Diagnosis of HCM typically involves a physical exam, imaging tests such as echocardiography, and genetic testing to identify any genetic mutations that may be causing the condition. Treatment for HCM may include medications to improve heart function, such as beta-blockers or calcium channel blockers, and surgery to remove part of the thickened heart muscle if necessary. In some cases, the implantation of a cardiac defibrillator may be recommended to prevent sudden cardiac death.
If you or someone you know is experiencing symptoms of HCM, it is important to speak with a healthcare provider for an accurate diagnosis and appropriate treatment. With proper management, people with HCM can lead normal, healthy lives, but regular monitoring and treatment are necessary to prevent serious complications.
Research Papers
Disease Signs and Symptoms
- Chest pain
- Fainting (syncope)
- Irregular heart sound (heart murmur)
- Rapid fluttering heartbeats (palpitations)
- Irregular heartbeats (arrhythmia)
- Shortness of breath (dyspnea)
- Difficulty breathing (dyspnea)
- Fainting, especially during or just after exercise or exertion
- Shortness of breath, especially during exercise
Disease Causes
Hypertrophic cardiomyopathy
Hypertrophic cardiomyopathy is usually caused by abnormal genes (gene mutations) that cause the heart muscle to grow abnormally thick.
In most people with hypertrophic cardiomyopathy, the muscular wall (septum) between the two bottom chambers of the heart (ventricles) becomes thicker than normal. As a result, the thicker wall may block blood flow out of the heart. This is called obstructive hypertrophic cardiomyopathy.
If there's no significant blocking of blood flow, the condition is called nonobstructive hypertrophic cardiomyopathy. However, the heart's main pumping chamber (left ventricle) may become stiff. This makes it hard for the heart to relax and reduces the amount of blood the ventricle can hold and send to the body with each heartbeat.
People with hypertrophic cardiomyopathy also have an abnormal arrangement of heart muscle cells (myofiber disarray). This can trigger arrhythmias in some people.
Disease Prevents
Hypertrophic cardiomyopathy
There is no known prevention for hypertrophic cardiomyopathy. But it's important to identify the condition as early as possible to guide treatment and prevent complications.
If you have a first-degree relative — a parent, sibling or child — with hypertrophic cardiomyopathy, doctors may recommend genetic testing to screen for the condition. However, not everyone with HCM has a currently detectable mutation. Also, some insurance companies may not cover genetic testing.
If genetic testing isn't done, or if the results aren't helpful, then your doctor may recommend echocardiograms on a regular basis if you have a family member with hypertrophic cardiomyopathy. Adolescents and competitive athletes should be screened once a year. Adults who don't compete in athletics should be screened every five years.
Disease Treatments
The goal of hypertrophic cardiomyopathy treatment is to relieve symptoms and prevent sudden cardiac death in people at high risk. Your specific treatment depends on the severity of your symptoms. Together, you and your doctor will discuss the most appropriate treatment for your condition.
Medications
Medications can help reduce how strong the heart muscle squeezes and slow the heart rate so that the heart can pump blood better. Medications to treat hypertrophic cardiomyopathy and its symptoms may include:
- Beta blockers such as metoprolol (Lopressor, Toprol-XL), propranolol (Inderal, Innopran XL) or atenolol (Tenormin)
- Calcium channel blockers such as verapamil (Verelan, Calan SR,) or diltiazem (Cardizem, Tiazac)
- Heart rhythm drugs such as amiodarone (Pacerone) or disopyramide (Norpace)
- Blood thinners such as warfarin (Coumadin, Jantoven), dabigatran (Pradaxa), rivaroxaban (Xarelto) or apixaban (Eliquis) to prevent blood clots if you have atrial fibrillation
Surgeries or other procedures
Several different surgeries or procedures are available to treat cardiomyopathy or its symptoms. They range from open-heart surgery to implantation of a device to control your heart rhythm.
- Septal myectomy. This open-heart surgery may be recommended if medications do not improve your symptoms. It involves removing part of the thickened, overgrown wall (septum) between the heart chambers. Septal myectomy helps improve blood flow out of the heart and reduces backward flow of blood through the mitral valve (mitral regurgitation).
- The surgery may be done using different approaches, depending on the location of the thickened heart muscle. In one type, called apical myectomy, surgeons remove thickened heart muscle from near the tip of the heart. Sometimes the mitral valve is repaired at the same time.
- Septal ablation. This procedure destroys the thickened heart muscle with alcohol. The alcohol is injected through a long, thin tube (catheter) into the artery supplying blood to that area. Possible complications include disruption of the heart's electrical system (heart block), which requires implantation of a pacemaker.
- Implantable cardioverter-defibrillator (ICD). An ICD is a small device that continuously monitors your heartbeat. It's implanted in your chest like a pacemaker. If a life-threatening arrhythmia occurs, the ICD delivers precisely calibrated electrical shocks to restore a normal heart rhythm. ICD has been shown to help prevent sudden cardiac death, which occurs in a small number of people with hypertrophic cardiomyopathy.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Hypertrophic cardiomyopathy and Learn More about Diseases

Klinefelter syndrome

Posterior vaginal prolapse (Rectocele)

Bladder exstrophy
Neuroblastoma
Sarcoma

Pancreatitis
Autoimmune pancreatitis

Delirium
hypertrophic cardiomyopathy, হাইপারট্রফিক কার্ডিওমায়োপ্যাথি
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.