 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
HPV infection

Oppositional defiant disorder (ODD) is a mental health disorder that primarily affects children and adolescents. It is characterized by a persistent pattern of disobedient, hostile, and defiant behavior toward authority figures, such as parents, teachers, and other adults.
The symptoms of ODD may include frequent temper tantrums, arguing with adults, deliberately disobeying rules, blaming others for one's own mistakes, and engaging in spiteful or vindictive behavior. These behaviors often lead to significant problems at home, school, and in other settings.
The exact causes of ODD are not fully understood, but a combination of genetic, environmental, and social factors may play a role. Risk factors for ODD may include a family history of ODD or other mental health disorders, a traumatic or stressful life event, or a dysfunctional family environment.
Treatment for ODD typically involves therapy, such as cognitive-behavioral therapy or family therapy, which can help children and their families develop better communication and problem-solving skills. In some cases, medication may also be prescribed to help manage symptoms such as impulsivity, irritability, or anxiety.
Early intervention and treatment for ODD can be very effective in helping children and adolescents learn how to manage their behavior and improve their relationships with others. It is important to seek professional help if you suspect your child may be struggling with ODD or any other mental health disorder.
Research Papers
Disease Signs and Symptoms
- Genital wart
- In most cases, common warts are simply unsightly, but they can also be painful or susceptible to injury or bleeding.
- Plantar warts are hard, grainy growths that usually appear on the heels or balls of your feet.
- These warts might cause discomfort.
Disease Causes
HPV infection
HPV infection occurs when the virus enters your body, usually through a cut, abrasion or small tear in your skin. The virus is transferred primarily by skin-to-skin contact.
Genital HPV infections are contracted through sexual intercourse, anal sex and other skin-to-skin contact in the genital region. Some HPV infections that result in oral or upper respiratory lesions are contracted through oral sex.
If you're pregnant and have an HPV infection with genital warts, it's possible your baby may get the infection. Rarely, the infection may cause a noncancerous growth in the baby's voice box (larynx).
Warts are contagious. They can spread through direct contact with a wart. Warts can also spread when someone touches something that already touched a wart.
Disease Prevents
HPV infection
Common warts
It's difficult to prevent HPV infections that cause common warts. If you have a common wart, you can prevent the spread of the infection and formation of new warts by not picking at a wart and not biting your nails.
Plantar warts
To reduce the risk of contracting HPV infections that cause plantar warts, wear shoes or sandals in public pools and locker rooms.
Genital warts
You can reduce your risk of developing genital warts and other HPV-related genital lesions by:
- Being in a mutually monogamous sexual relationship
- Reducing your number of sex partners
- Using a latex condom, which can reduce your risk of HPV transmission
HPV vaccines
Gardasil 9 is an HPV vaccine approved by the U.S. Food and Drug Administration and can be used for males and females to protect against cervical cancer and genital warts.
The Centers for Disease Control and Prevention (CDC) recommends routine HPV vaccination for girls and boys ages 11 and 12, although it can be given as early as age 9. It's ideal for girls and boys to receive the vaccine before they have sexual contact and are exposed to HPV. Research has shown that receiving the vaccine at a young age isn't linked to an earlier start of sexual activity.
Once someone is infected with HPV, the vaccine might not be as effective or might not work at all. Also, response to the vaccine is better at younger ages than older ones. But, if given before someone is infected, the vaccine can prevent most cases of cervical cancer.
The CDC recommends that all 11- and 12-year-olds receive two doses of HPV vaccine at least six months apart. Younger adolescents ages 9 and 10 and teens ages 13 and 14 can also receive vaccination on the updated two-dose schedule. Research has shown that the two-dose schedule is effective for children under 15.
Teens and young adults who begin the vaccine series later, at ages 15 through 26, should continue to receive three doses of the vaccine.
The CDC recommends catch-up HPV vaccinations for all people through age 26 who aren't adequately vaccinated.
The U.S. Food and Drug Administration recently approved the use of Gardasil 9 for males and females ages 9 to 45. If you're age 27 to 45, discuss with your doctor whether he or she recommends that you get the HPV vaccine.
Disease Treatments
Warts often go away without treatment, particularly in children. However, there's no cure for the virus, so they can reappear in the same place or other places.
Medications
Medications to eliminate warts are typically applied directly to the lesion and usually take many applications before they're successful. Examples include:
- Salicylic acid. Over-the-counter treatments that contain salicylic acid work by removing layers of a wart a little at a time. For use on common warts, salicylic acid can cause skin irritation and isn't for use on your face.
- Imiquimod. This prescription cream might enhance your immune system's ability to fight HPV. Common side effects include redness and swelling at the application site.
- Podofilox. Another topical prescription, podofilox works by destroying genital wart tissue. Podofilox may cause burning and itching where it's applied.
- Trichloroacetic acid. This chemical treatment burns off warts on the palms, soles and genitals. It might cause local irritation.
Surgical and other procedures
If medications don't work, your doctor might suggest removing warts by one of these methods:
- Freezing with liquid nitrogen (cryotherapy)
- Burning with an electrical current (electrocautery)
- Surgical removal
- Laser surgery
Treatment for HPV in the cervix
If you have an abnormal HPV or Pap test, your gynecologist will perform a procedure called a colposcopy. Using an instrument that provides a magnified view of the cervix (colposcope), your doctor will look closely at the cervix and take samples (biopsy) of any areas that look abnormal.
Any precancerous lesions need to be removed. Options include freezing (cryosurgery), laser, surgical removal, loop electrosurgical excision procedure (LEEP) and cold knife conization. LEEP uses a thin looped wire charged with an electric current to remove a thin layer of a section of the cervix and cold knife conization is a surgical procedure that removes a cone-shaped piece of the cervix.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
HPV infection and Learn More about Diseases

Pinched nerve

Primary immunodeficiency

Granuloma annulare
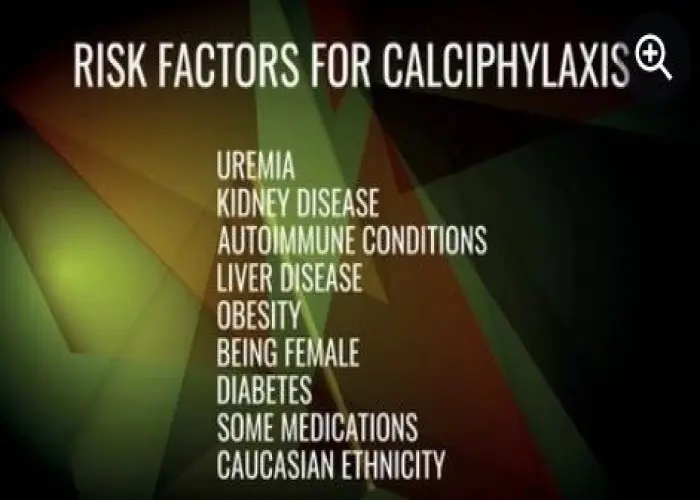
Calciphylaxis

Radiation sickness
Chronic lymphocytic leukemia

Heart attack
Pulmonary hypertension
HPV infection, oppositional defiant disorder, odd, এইচপিভি সংক্রমণ, অপজিশনাল ডিফিয়েন্ট ডিসঅর্ডার, ওডিডি
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
