 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Hemochromatosis

Hemochromatosis is a condition in which there is an excess buildup of iron in the body, which can lead to damage to various organs and tissues. It is an inherited disorder, and in most cases is caused by a mutation in a gene that regulates iron absorption and storage.
Iron overload can cause a variety of symptoms, including fatigue, joint pain, abdominal pain, and darkening of the skin. Over time, it can lead to more serious complications, such as liver damage, diabetes, and heart problems.
Hemochromatosis can be diagnosed through blood tests that measure the level of iron in the blood, as well as genetic testing to look for the specific gene mutations associated with the condition. Treatment for hemochromatosis typically involves regular phlebotomy, a procedure in which blood is drawn to reduce the amount of iron in the body. In some cases, medication may be prescribed to help remove excess iron from the body.
Early diagnosis and treatment of hemochromatosis are important in order to prevent or manage potential complications. If you have a family history of hemochromatosis or are experiencing symptoms that may be related to iron overload, it is important to see a healthcare provider for evaluation and testing.
Research Papers
Disease Signs and Symptoms
- Joint pain
- Liver failure
- Heart failure
- Impotence
- Reduced sexual desire
- Diabetes
- Weakness
- Fatigue (Tiredness)
- Abdomen pain
- Memory loss
Disease Causes
Hemochromatosis
Hereditary hemochromatosis is caused by a mutation in a gene that controls the amount of iron your body absorbs from the food you eat. These mutations are passed from parents to children. This type of hemochromatosis is by far the most common type.
Gene mutations that cause hemochromatosis
A gene called HFE is most often the cause of hereditary hemochromatosis. You inherit one HFE gene from each of your parents. The HFE gene has two common mutations, C282Y and H63D. Genetic testing can reveal whether you have these mutations in your HFE gene.
- If you inherit 2 abnormal genes, you may develop hemochromatosis. You can also pass the mutation on to your children. But not everyone who inherits two genes develops problems linked to the iron overload of hemochromatosis.
- If you inherit 1 abnormal gene, you're unlikely to develop hemochromatosis. However, you are considered a gene mutation carrier and can pass the mutation on to your children. But your children wouldn't develop the disease unless they also inherited another abnormal gene from the other parent.
How hemochromatosis affects your organs
Iron plays an essential role in several body functions, including helping in the formation of blood. But too much iron is toxic.
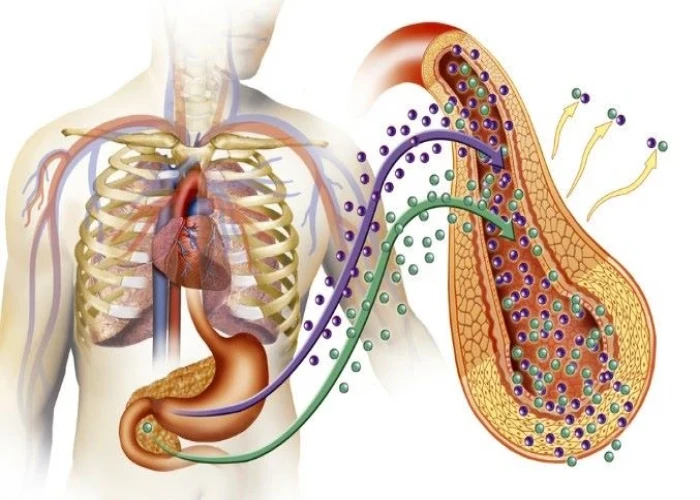
A hormone called hepcidin, secreted by the liver, normally controls how iron is used and absorbed in the body, as well as how excess iron is stored in various organs. In hemochromatosis, the normal role of hepcidin is disrupted, causing your body to absorb more iron than it needs.
This excess iron is stored in major organs, especially your liver. Over a period of years, the stored iron can cause severe damage that may lead to organ failure and chronic diseases, such as cirrhosis, diabetes and heart failure. Though many people have faulty genes that cause hemochromatosis, not everyone develops iron overload to a degree that causes tissue and organ damage.
Hereditary hemochromatosis isn't the only type of hemochromatosis. Other types include:
- Juvenile hemochromatosis. This causes the same problems in young people that hereditary hemochromatosis causes in adults. But iron accumulation begins much earlier, and symptoms usually appear between the ages of 15 and 30. This disorder is caused by mutations in the hemojuvelin or hepcidin genes.
- Neonatal hemochromatosis. In this severe disorder, iron builds up rapidly in the liver of the developing baby in the womb. It is thought to be an autoimmune disease, in which the body attacks itself.
- Secondary hemochromatosis. This form of the disease is not inherited and is often referred to as iron overload. People with certain types of anemia or chronic liver disease may need multiple blood transfusions, which can lead to excess iron accumulation.
Disease Prevents
Disease Treatments
Blood removal
Doctors can treat hereditary hemochromatosis safely and effectively by removing blood from your body (phlebotomy) on a regular basis, just as if you were donating blood.
The goal of phlebotomy is to reduce your iron levels to normal. The amount of blood removed and how often it's removed depend on your age, your overall health and the severity of iron overload.
- Initial treatment schedule. Initially, you may have a pint (about 470 milliliters) of blood taken once or twice a week — usually in a hospital or your doctor's office. While you recline in a chair, a needle is inserted into a vein in your arm. The blood flows from the needle into a tube that's attached to a blood bag.
- Maintenance treatment schedule. Once your iron levels have returned to normal, blood can be removed less often, typically every two to three months. Some people may maintain normal iron levels without having any blood taken, and some may need to have blood removed monthly. The schedule depends on how rapidly iron accumulates in your body.
Treating hereditary hemochromatosis can help alleviate symptoms of tiredness, abdominal pain and skin darkening. It can help prevent serious complications such as liver disease, heart disease and diabetes. If you already have one of these conditions, phlebotomy may slow the progression of the disease, and in some cases even reverse it.
Phlebotomy will not reverse cirrhosis or joint pain, but it can slow the progression.
If you have cirrhosis, your doctor may recommend periodic screening for liver cancer. This usually involves an abdominal ultrasound and CT scan.
Chelation for those who can't undergo blood removal
If you can't undergo phlebotomy, because you have anemia, for example, or heart complications, your doctor may recommend a medication to remove excess iron. The medication can be injected into your body, or it can be taken as a pill. The medication binds excess iron, allowing your body to expel iron through your urine or stool in a process that's called chelation (KEE-lay-shun). Chelation is not commonly used in hereditary hemochromatosis.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Hemochromatosis and Learn More about Diseases
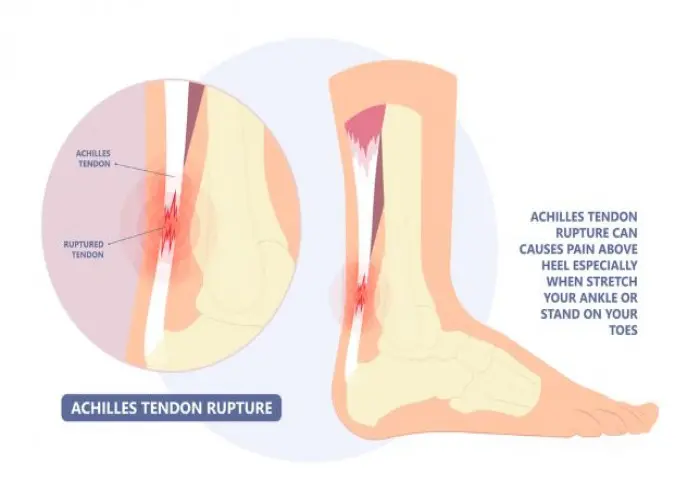
Achilles tendon rupture

Hemophilia

Deep vein thrombosis (DVT)
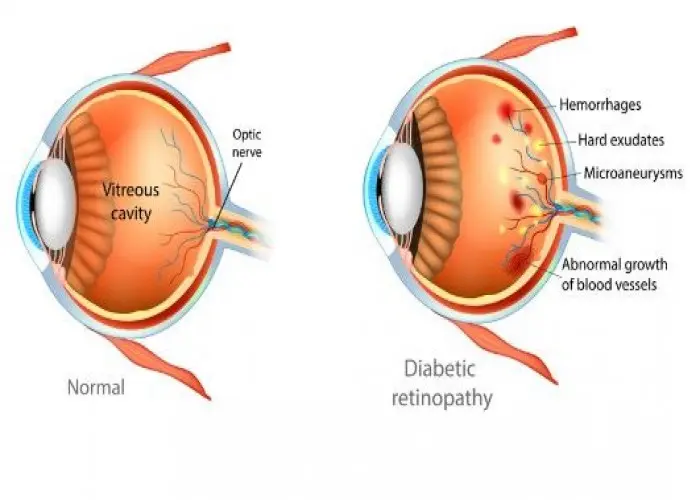
Diabetic retinopathy
Epiglottitis

Jaundice
Pheochromocytoma

Keloid scar
hemochromatosis, হিমোক্রোমাটোসিস
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
