Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
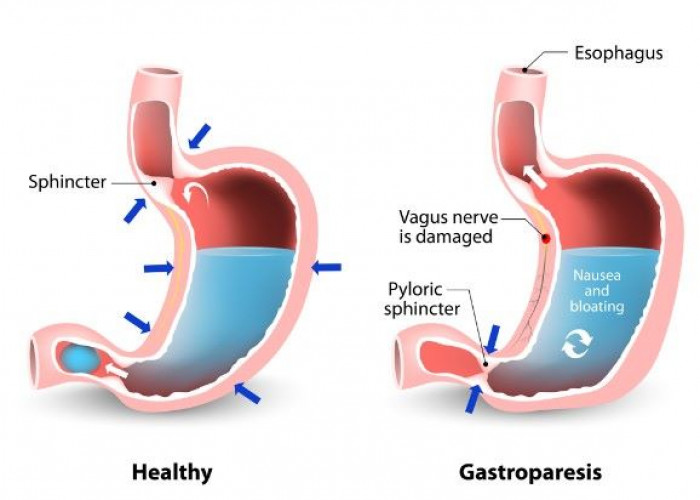
Gastroparesis
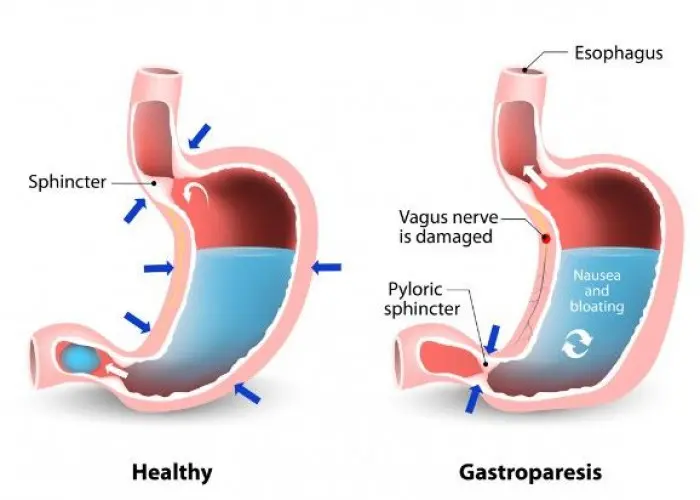
Gastroparesis is a medical condition that affects the normal movement of food from the stomach to the small intestine. It is caused by damage to the nerves that control the stomach muscles or damage to the muscles themselves. This can result in delayed emptying of the stomach, which can cause a variety of symptoms.
The most common symptoms of gastroparesis include:
- Nausea
- Vomiting
- Abdominal pain or discomfort
- Feeling full after eating only a small amount of food
- Bloating
- Acid reflux
Gastroparesis can be caused by a variety of factors, including diabetes, nervous system disorders, surgery, certain medications, and viral infections. The condition is more common in women than in men.
Diagnosis of gastroparesis may involve a physical exam, medical history, and diagnostic tests such as gastric emptying studies, which measure how quickly food leaves the stomach. Treatment for gastroparesis may involve dietary changes, such as eating smaller, more frequent meals or avoiding high-fat or high-fiber foods, or medications to promote stomach contractions or reduce nausea and vomiting. In more severe cases, a healthcare professional may recommend surgery to remove the damaged portion of the stomach or implant a device to stimulate stomach muscles.
If left untreated, gastroparesis can lead to complications such as malnutrition, dehydration, or bacterial overgrowth in the small intestine. If you are experiencing symptoms of gastroparesis, it is important to seek medical attention for an accurate diagnosis and appropriate treatment.
Research Papers
Disease Signs and Symptoms
- Nausea or vomiting
- Abdomen bloating
- Abdomen pain
- Early fullness during a meal
- Acid regurgitation
- Changes in blood sugar levels
- Loss of appetite
- Weight loss
Disease Causes
Gastroparesis
It's not always clear what leads to gastroparesis, but in some cases it can be caused by damage to a nerve that controls the stomach muscles (vagus nerve).
The vagus nerve helps manage the complex processes in your digestive tract, including signaling the muscles in your stomach to contract and push food into the small intestine. A damaged vagus nerve can't send signals normally to your stomach muscles. This may cause food to remain in your stomach longer, rather than move into your small intestine to be digested.
The vagus nerve and its branches can be damaged by diseases, such as diabetes, or by surgery to the stomach or small intestine.
Disease Prevents
Disease Treatments
Treating gastroparesis begins with identifying and treating the underlying condition. If diabetes is causing your gastroparesis, your doctor can work with you to help you control it.
Changes to your diet
Maintaining adequate nutrition is the most important goal in the treatment of gastroparesis. Many people can manage gastroparesis with dietary changes. Your doctor may refer you to a dietitian who can work with you to find foods that are easier for you to digest. This can help you to get enough calories and nutrients from the food you eat.
A dietitian might suggest that you try to:
- Eat smaller meals more frequently
- Chew food thoroughly
- Eat well-cooked fruits and vegetables rather than raw fruits and vegetables
- Avoid fibrous fruits and vegetables, such as oranges and broccoli, which may cause bezoars
- Choose mostly low-fat foods, but if you can tolerate fat, add small servings of fatty foods to your diet
- Try soups and pureed foods if liquids are easier for you to swallow
- Drink about 34 to 51 ounces (1 to 1.5 liters) of water a day
- Exercise gently after you eat, such as going for a walk
- Avoid carbonated drinks, alcohol and smoking
- Try to avoid lying down for two hours after a meal
- Take a multivitamin daily
Ask your dietitian for a comprehensive list of foods recommended for people with gastropareses. Here's a brief list:
Starches
- White bread and rolls and whole-wheat bread without nuts or seeds
- Plain or egg bagels
- English muffins
- Flour or corn tortillas
- Pancakes
- Puffed wheat and rice cereals
- Cream of Wheat or rice
- White crackers
- Potatoes, white or sweet (no skin)
- Baked french fries
- Rice
- Pasta
Protein
- Lean beef, veal and pork (not fried)
- Chicken or turkey (no skin and not fried)
- Crab, lobster, shrimp, clams, scallops, oysters
- Tuna (packed in water)
- Cottage cheese
- Eggs
- Tofu
- Strained meat baby food
Fruits and vegetables
- Pureed vegetables and fruits, such as baby food
- Tomato sauce, paste, puree, juice
- Carrots (cooked)
- Beets (cooked)
- Mushrooms (cooked)
- Vegetable juice
- Vegetable broth
- Fruit juices and drinks
- Applesauce
- Bananas
- Peaches and pears (canned)
Dairy
- Milk, if tolerated
- Yogurt (without fruit pieces)
- Custard and pudding
- Frozen yogurt
Medications
Medications to treat gastroparesis may include:
- Medications to stimulate the stomach muscles. These medications include metoclopramide (Reglan) and erythromycin. Metoclopramide has a risk of serious side effects. Erythromycin may lose its effectiveness over time, and can cause side effects, such as diarrhea.
- A newer medication, domperidone, with fewer side effects, is also available with restricted access.
- Medications to control nausea and vomiting. Drugs that help ease nausea and vomiting include diphenhydramine (Benadryl, others) and ondansetron (Zofran). Prochlorperazine (Compro) is used if nausea and vomiting persist.
Surgical treatment
Some people with gastroparesis may be unable to tolerate any food or liquids. In these situations, doctors may recommend a feeding tube (jejunostomy tube) be placed in the small intestine. Or doctors may recommend a gastric venting tube to help relieve pressure from gastric contents.
Feeding tubes can be passed through your nose or mouth or directly into your small intestine through your skin. The tube is usually temporary and is only used when gastroparesis is severe or when blood sugar levels can't be controlled by any other method. Some people may require an IV (parenteral) feeding tube that goes directly into a vein in the chest.
Treatments under investigation
Researchers are continuing to investigate new medications to treat gastroparesis.
One example is a new drug in development called Relamorelin. The results of a phase II trial found the drug could speed up gastric emptying and reduce vomiting. The drug is not yet approved in the United States by the Food and Drug Administration (FDA), but a larger clinical trial is currently underway.
A number of new therapies are being tried with the help of endoscopy — a procedure done with a slender tube (endoscope) that's threaded down the esophagus.
One procedure, known as endoscopic pyloromyotomy (gastric peroral endoscopic myotomy, or G-POEM), involves making an incision in the valve or muscular ring between the stomach and small intestine called the pylorus. A channel is then opened from the stomach to the small intestine. This is a relatively recent procedure that shows promise, though additional research is needed.
Another type of endoscopic procedure involves placing a small tube (stent) where the stomach connects to the small intestine (duodenum) to keep this connection open.
Gastric electrical stimulation and pacing
In gastric electrical stimulation, a surgically implanted device provides electrical stimulation to the stomach muscles to move food more efficiently. Study results have been mixed. However, the device seems to be most helpful for people with diabetic gastroparesis.
The FDA allows the device to be used under a compassionate use exemption for those who can't control their gastroparesis symptoms with diet changes or medications. However, larger studies are needed.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Gastroparesis and Learn More about Diseases

Toe walking in children

Ameloblastoma

Castleman disease

Male breast cancer

Immune thrombocytopenia (ITP)

Yellow fever
Myocardial ischemia

Snake bite
gastroparesis, গ্যাস্ট্রোপারেসিস
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.