 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Vulvar cancer

Vulvar cancer is a type of cancer that affects the external female genitalia, including the labia, clitoris, and vaginal opening. It is relatively rare, accounting for less than 5% of all gynecologic cancers.
The most common symptom of vulvar cancer is a persistent lump or sore on the vulva, which may be painful or itchy. Other symptoms can include changes in the skin color or texture of the vulva, bleeding or discharge not related to menstruation, and pain during sexual intercourse or urination.
The exact causes of vulvar cancer are not fully understood, but certain factors can increase the risk of developing the disease, including human papillomavirus (HPV) infection, smoking, a history of precancerous conditions of the vulva, and a weakened immune system.
Diagnosis of vulvar cancer typically involves a physical exam, including a pelvic exam, and a biopsy to examine a sample of tissue from the affected area. Imaging tests, such as ultrasound, CT or MRI scans, may also be used to determine the extent of the cancer.
Treatment for vulvar cancer depends on the stage and extent of the disease, but may include surgery to remove the affected tissue, radiation therapy, and chemotherapy. In some cases, a combination of these treatments may be used. If the cancer is detected early, it is often curable with surgery alone.
After treatment, ongoing follow-up care and monitoring is important to detect any potential recurrences or complications. This may include regular pelvic exams, imaging tests, and blood tests to monitor for any signs of cancer.
Research Papers
Disease Signs and Symptoms
- Vaginal itching
- Heavy menstrual period or bleeding
- Skin is thick
- Ulcer
- A lump, wartlike bumps or an open sore (ulcer)
- Vaginal cancer
Disease Causes
Vulvar cancer
It's not clear what causes vulvar cancer.
In general, doctors know that cancer begins when a cell develops changes (mutations) in its DNA. The DNA contains the instructions that tell a cell what to do. The mutations tell the cell to grow and divide rapidly. The cell and its offspring go on living when other normal cells would die. The accumulating cells form a tumor that may be cancerous, invading nearby tissue and spreading to other parts of the body.
Types of vulvar cancer
The type of cell in which vulvar cancer begins helps your doctor plan the most effective treatment. The most common types of vulvar cancer include:
- Vulvar squamous cell carcinoma. This cancer begins in the thin, flat cells that line the surface of the vulva. Most vulvar cancers are squamous cell carcinomas.
- Vulvar melanoma. This cancer begins in the pigment-producing cells found in the skin of the vulva.
Disease Prevents
Vulvar cancer
Reduce your risk of sexually transmitted infections
To reduce your risk of vulvar cancer, reduce your risk of the sexually transmitted infection HPV:
- Use a condom every time you have sex. Condoms may reduce your risk of contracting HPV but can't fully protect against it.
- Get the HPV vaccine. Children and young adults may consider the HPV vaccine, which protects against the strains of the virus that are thought to cause the most cases of vulvar cancer.
Ask your doctor about pelvic exams
Ask your doctor how often you should undergo pelvic exams. These exams allow your doctor to visually examine your vulva and manually examine your internal reproductive organs to check for abnormalities.
Talk to your doctor about your risk factors for vulvar cancer and other pelvic cancers in order to determine the most appropriate screening exam schedule for you.
Disease Treatments
Treatment options for vulvar cancer depend on the type, stage and location of your cancer, as well as your overall health and your preferences.
Surgery
Operations used to treat vulvar cancer include:
- Removing the cancer and a margin of healthy tissue (excision). This procedure, which may also be called a wide local excision or radical excision, involves cutting out the cancer and a small amount of normal tissue that surrounds it. Cutting out what doctors refer to as a margin of normal-looking tissue helps ensure that all of the cancerous cells have been removed.
- Removing part of the vulva or the entire vulva (vulvectomy). Surgery to remove part of the vulva (partial vulvectomy) or the entire vulva, including the underlying tissue (radical vulvectomy), may be an option for larger cancers. People with larger cancers may also consider treatment that combines radiation therapy and chemotherapy to shrink the tumor before surgery, which may allow for a less extensive operation.
- Removing a few nearby lymph nodes (sentinel node biopsy). To determine whether cancer has spread to the lymph nodes, the surgeon may use a procedure called sentinel node biopsy. This procedure identifies the lymph nodes most likely to contain cancer so they can be removed and analyzed. If cancer isn't found in those first lymph nodes, it's unlikely to be in any other lymph nodes.
- Removing many lymph nodes. If the cancer has spread to the lymph nodes, many lymph nodes may be removed to reduce the risk that cancer will spread to distant areas of the body.
Surgery carries a risk of complications, such as infection and problems with healing around the incision. Removing lymph nodes can cause fluid retention and leg swelling, a condition called lymphedema.
Radiation therapy
Radiation therapy uses high-powered energy beams, such as X-rays and protons, to kill cancer cells. Radiation therapy for vulvar cancer is usually administered by a machine that moves around your body and directs radiation to precise points on your skin (external beam radiation).
Radiation therapy is sometimes used to shrink large vulvar cancers in order to make it more likely that surgery will be successful. Radiation therapy is sometimes combined with chemotherapy, which can make cancer cells more vulnerable to the radiation.
If cancer cells are discovered in your lymph nodes, your doctor may recommend radiation to the area around your lymph nodes to kill any cancer cells that might remain after surgery. Radiation is sometimes combined with chemotherapy in these situations.
Chemotherapy
Chemotherapy is a drug treatment that uses chemicals to kill cancer cells. Chemotherapy drugs are typically administered through a vein in your arm or by mouth.
For those with advanced vulvar cancer that has spread to other areas of the body, chemotherapy may be an option.
Chemotherapy is sometimes combined with radiation therapy to shrink large vulvar cancers in order to make it more likely that surgery will be successful. Chemotherapy may also be combined with radiation to treat cancer that has spread to the lymph nodes.
Targeted drug therapy
Targeted drug treatments focus on specific abnormalities present within cancer cells. By blocking these abnormalities, targeted drug treatments can cause cancer cells to die.
Targeted therapy might be an option for treating advanced vulvar cancer.
Immunotherapy
Immunotherapy uses your immune system to fight cancer. Your body's disease-fighting immune system may not attack your cancer because the cancer cells produce proteins that help them hide from the immune system cells. Immunotherapy works by interfering with that process.
Immunotherapy might be an option for treating advanced vulvar cancer.
Follow-up tests after treatment
After completing vulvar cancer treatment, your doctor may recommend periodic follow-up exams to look for a cancer recurrence. Even after successful treatment, vulvar cancer can return. Your doctor will determine the schedule of follow-up exams that's right for you, but doctors generally recommend exams two to four times each year for the first two years after vulvar cancer treatment.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
-
Calcarea fluorica
200, 1000 power.
-
Lapis albus
3, 6 strength.
- Carbo animalis
- Carbo vegetabilis
- Kreosotum
- Bromium
- Baryta carbonica
- Silicea
- Calcarea iodata
- Sulphur
- Arsenicum
- Graphites
Disease yoga
Vulvar cancer and Learn More about Diseases
Carotid artery disease
Congenital adrenal hyperplasia

Dog Bite

Adult Stills disease

Conjoined twins
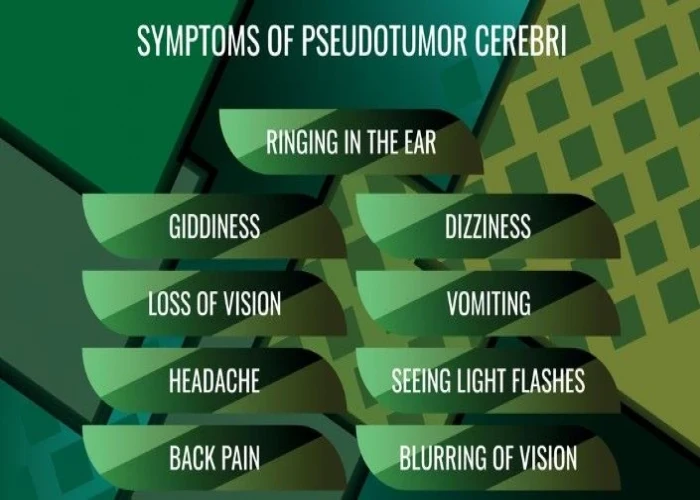
Pseudotumor cerebri (idiopathic intracranial hypertension)

Sleepwalking
Sex headaches
vulvar cancer, ভলভার ক্যান্সার
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
