Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Fetal macrosomia
Fetal macrosomia is a condition in which a fetus grows larger than average, typically weighing over 4,000 grams (8 pounds, 13 ounces) at birth. While some babies are just naturally large, fetal macrosomia is usually the result of maternal factors such as gestational diabetes, obesity, or a family history of large babies.
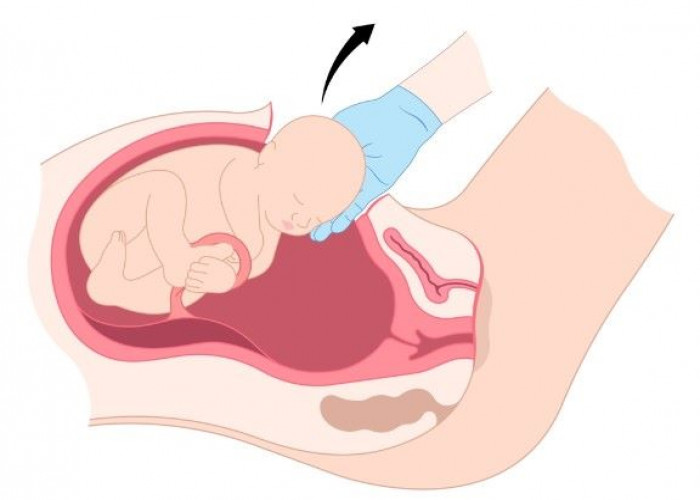
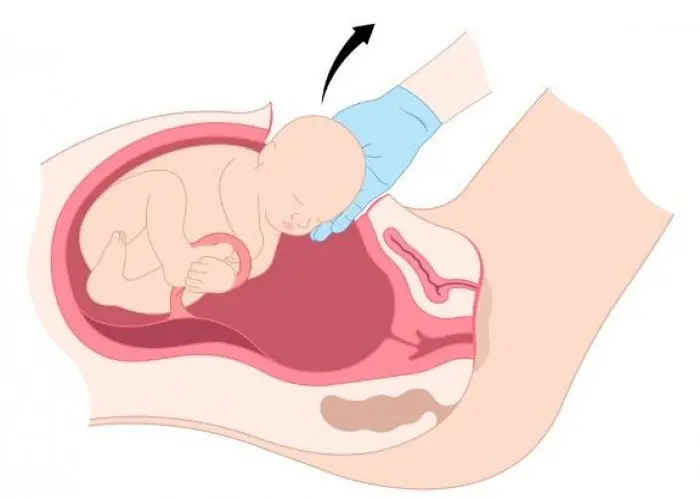
Fetal macrosomia can increase the risk of complications during pregnancy and delivery. For example, it can make it more difficult for the baby to pass through the birth canal, increasing the risk of shoulder dystocia (when the baby's shoulder becomes stuck behind the mother's pubic bone), birth injuries such as fractures or nerve damage, and the need for a cesarean section delivery.
In addition, babies with fetal macrosomia are at higher risk of certain health problems after birth, such as low blood sugar, respiratory distress, and jaundice.
To reduce the risk of complications, healthcare providers may monitor mothers with risk factors for fetal macrosomia more closely during pregnancy and delivery. This may include more frequent ultrasounds to monitor fetal growth, blood sugar monitoring for gestational diabetes, and consideration of a scheduled c-section if the baby is estimated to be very large. In some cases, induction of labor may be recommended to avoid prolonged labor or other complications associated with vaginal delivery.
Research Papers
Disease Signs and Symptoms
- Excessive amniotic fluid (polyhydramnios)
Disease Causes
Fetal macrosomia
Genetic factors and maternal conditions such as obesity or diabetes can cause fetal macrosomia. Rarely, a baby might have a medical condition that makes him or her grow faster and larger.
Sometimes it's unknown what causes a baby to be larger than average.
Disease Prevents
Fetal macrosomia
You might not be able to prevent fetal macrosomia, but you can promote a healthy pregnancy. Research shows that exercising during pregnancy and eating a low-glycemic diet can reduce the risk of macrosomia.
For example:
- Schedule a preconception appointment. If you're considering pregnancy, talk with your health care provider. If you're obese, you might also be referred to another health care provider — such as a registered dietitian or an obesity specialist — who can help you reach a healthy weight before pregnancy.
- Monitor your weight. Gaining a healthy amount of weight during pregnancy — often 25 to 35 pounds (about 11 to 16 kilograms) if you have a normal pre-pregnancy weight — supports your baby's growth and development. Women who weigh more when they get pregnant will have lower recommended pregnancy weight gain. Work with your health care provider to determine what's right for you.
- Manage diabetes. If you had diabetes before pregnancy or if you develop gestational diabetes, work with your health care provider to manage the condition. Controlling your blood sugar level is the best way to prevent complications, including fetal macrosomia.
- Be active. Follow your health care provider's recommendations for physical activity.
Disease Treatments
When it's time for your baby to be born, a vaginal delivery won't necessarily be out of the question. Your health care provider will discuss options as well as risks and benefits. He or she will monitor your labor closely for possible signs of a complicated vaginal delivery.
Inducing labor — stimulating uterine contractions before labor begins on its own — isn't generally recommended. Research suggests that labor induction doesn't reduce the risk of complications related to fetal macrosomia and might increase the need for a C-section.
Your health care provider might recommend a C-section if:
- You have diabetes. If you had diabetes before pregnancy or you develop gestational diabetes and your health care provider estimates that your baby weighs 9 pounds, 15 ounces (4,500 grams) or more, a C-section might be the safest way to deliver your baby.
- Your baby weighs 11 pounds or more and you don't have a history of maternal diabetes. If you don't have pre-gestational or gestational diabetes and your health care provider estimates that your baby weighs 11 pounds (5,000 grams) or more, a C-section might be recommended.
- You delivered a baby whose shoulder got stuck behind your pelvic bone (shoulder dystocia). If you've delivered one baby with shoulder dystocia, you're at increased risk of the problem occurring again. A C-section might be recommended to avoid the risks associated with shoulder dystocia, such as a fractured collarbone.
If your health care provider recommends an elective C-section, be sure to discuss the risks and benefits.
After your baby is born, he or she will likely be examined for signs of birth injuries, abnormally low blood sugar (hypoglycemia) and a blood disorder that affects the red blood cell count (polycythemia). He or she might need special care in the hospital's neonatal intensive care unit.
Keep in mind that your baby might be at risk of childhood obesity and insulin resistance and should be monitored for these conditions during future checkups.
Also, if you haven't previously been diagnosed with diabetes and your health care provider is concerned about the possibility of diabetes, you may be tested for the condition. During future pregnancies, you'll be closely monitored for signs and symptoms of gestational diabetes — a type of diabetes that develops during pregnancy.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Fetal macrosomia and Learn More about Diseases

Anorexia nervosa

Medication overuse headaches
Testicular cancer

Complicated grief

Mood disorders
Wolff-Parkinson-White (WPW) syndrome

Rickets

Gastritis
fetal macrosomia, ভ্রূণের ম্যাক্রোসোমিয়া
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.