Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
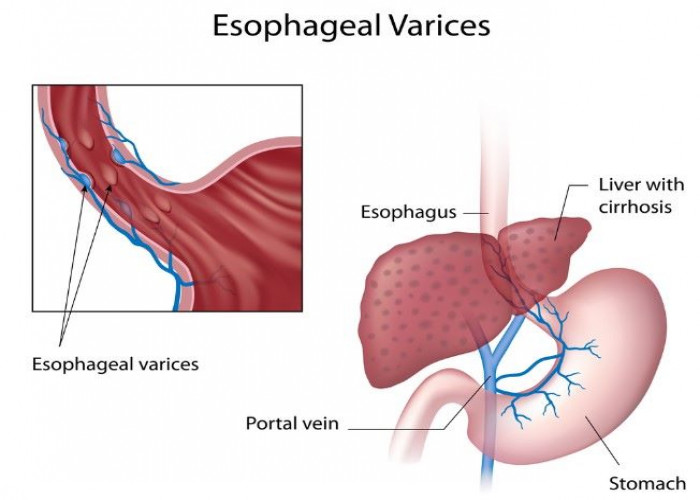
Esophageal varices
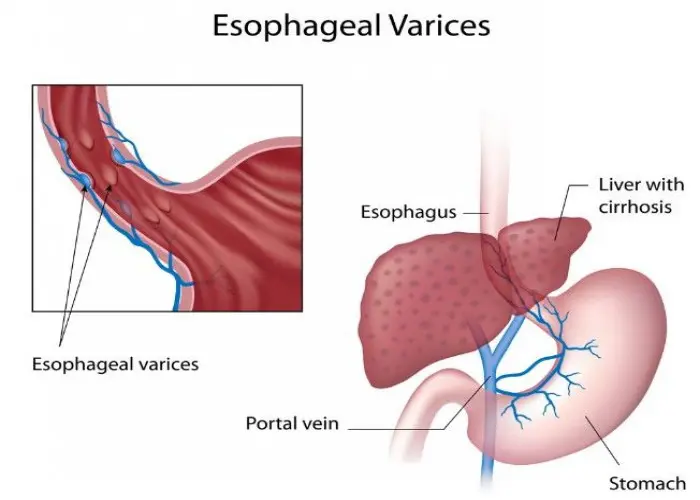
Esophageal varices are abnormally enlarged veins in the lower part of the esophagus, which is the muscular tube that connects the throat to the stomach. These veins are a common complication of liver disease, particularly cirrhosis, which is a condition where the liver becomes scarred and is unable to function properly.
In a healthy liver, blood flows from the digestive organs through the liver, where it is processed and filtered before flowing back into the body. When the liver is damaged, blood flow through the liver can become blocked or slowed down, causing pressure to build up in the veins that carry blood to the liver. This can lead to the development of esophageal varices, as the blood finds alternative pathways to return to the heart.
Esophageal varices can be dangerous, as they are prone to bleeding. If the veins rupture, it can cause severe bleeding in the digestive tract, which can be life-threatening if not treated promptly. Symptoms of esophageal varices include difficulty swallowing, vomiting blood, and dark, tarry stools.
Treatment for esophageal varices typically involves medications to reduce pressure in the veins, as well as procedures such as band ligation or sclerotherapy, which involve closing off the affected veins to prevent bleeding. In some cases, a liver transplant may be necessary to treat the underlying liver disease and prevent the development of new varices.
Research Papers
Disease Signs and Symptoms
- Nausea or vomiting
- Black, tarry or bloody stools
- Dizziness, lightheadedness or faintness
- Loss of consciousness (fainting)
- Yellowing of skin and eyes (jaundice)
- Excessive bruising
- Fluid buildup in abdomen (ascites)
Disease Causes
Esophageal varices
Esophageal varices sometimes form when blood flow to your liver is blocked, most often by scar tissue in the liver caused by liver disease. The blood flow begins to back up, increasing pressure within the large vein (portal vein) that carries blood to your liver.
This increased pressure (portal hypertension) forces the blood to seek other pathways through smaller veins, such as those in the lowest part of the esophagus. These thin-walled veins balloon with the added blood. Sometimes the veins rupture and bleed.
Causes of esophageal varices include:
- Severe liver scarring (cirrhosis). A number of liver diseases — including hepatitis infection, alcoholic liver disease, fatty liver disease and a bile duct disorder called primary biliary cirrhosis — can result in cirrhosis.
- Blood clot (thrombosis). A blood clot in the portal vein or in a vein that feeds into the portal vein (splenic vein) can cause esophageal varices.
- Parasitic infection. Schistosomiasis is a parasitic infection found in parts of Africa, South America, the Caribbean, the Middle East and East Asia. The parasite can damage the liver, as well as the lungs, intestine, bladder and other organs.
Disease Prevents
Esophageal varices
Currently, no treatment can prevent the development of esophageal varices in people with cirrhosis. While beta blocker drugs are effective in preventing bleeding in many people who have esophageal varices, they don't prevent esophageal varices from forming.
If you've been diagnosed with liver disease, ask your doctor about strategies to avoid liver disease complications. To keep your liver healthy:
- Don't drink alcohol. People with liver disease are often advised to stop drinking alcohol, since the liver processes alcohol. Drinking alcohol may stress an already vulnerable liver.
- Eat a healthy diet. Choose a plant-based diet that's full of fruits and vegetables. Select whole grains and lean sources of protein. Reduce the amount of fatty and fried foods you eat.
- Maintain a healthy weight. An excess amount of body fat can damage your liver. Obesity is associated with a greater risk of complications of cirrhosis. Lose weight if you are obese or overweight.
- Use chemicals sparingly and carefully. Follow the directions on household chemicals, such as cleaning supplies and insect sprays. If you work around chemicals, follow all safety precautions. Your liver removes toxins from your body, so give it a break by limiting the amount of toxins it must process.
- Reduce your risk of hepatitis. Sharing needles and having unprotected sex can increase your risk of hepatitis B and C. Protect yourself by abstaining from sex or using a condom if you choose to have sex. Get tested for exposure to hepatitis A, B and C, since infection can make your liver disease worse. Also ask your doctor whether you should be vaccinated for hepatitis A and hepatitis B.
Disease Treatments
The primary aim in treating esophageal varices is to prevent bleeding. Bleeding esophageal varices are life-threatening. If bleeding occurs, treatments are available to try to stop the bleeding.
Treatment to prevent bleeding
Treatments to lower blood pressure in the portal vein may reduce the risk of bleeding esophageal varices. Treatments may include:
- Medications to reduce pressure in the portal vein. A type of blood pressure drug called a beta blocker may help reduce blood pressure in your portal vein, decreasing the likelihood of bleeding. These medications include propranolol (Inderal, Innopran XL) and nadolol (Corgard).
- Using elastic bands to tie off bleeding veins. If your esophageal varices appear to have a high risk of bleeding, or if you've had bleeding from varices before, your doctor might recommend a procedure called endoscopic band ligation.
- Using an endoscope, the doctor uses suction to pull the varices into a chamber at the end of the scope and wraps them with an elastic band, which essentially "strangles" the veins so they can't bleed. Endoscopic band ligation carries a small risk of complications, such as bleeding and scarring of the esophagus.
Treatment if you're bleeding
Bleeding esophageal varices are life-threatening, and immediate treatment is essential. Treatments used to stop bleeding and reverse the effects of blood loss include:
- Using elastic bands to tie off bleeding veins. Your doctor may wrap elastic bands around the esophageal varices during an endoscopy.
- Medications to slow blood flow into the portal vein. Drugs such as octreotide (Sandostatin) and vasopressin (Vasostrict) slow the flow of blood to the portal vein. The drug is usually continued for up to five days after a bleeding episode.
- Diverting blood flow away from the portal vein. If medication and endoscopy treatments don't stop the bleeding, your doctor might recommend a procedure called transjugular intrahepatic portosystemic shunt (TIPS).
- The shunt is an opening that is created between the portal vein and the hepatic vein, which carries blood from your liver to your heart. The shunt reduces pressure in the portal vein and often stops bleeding from esophageal varices.
- But TIPS can cause serious complications, including liver failure and mental confusion, which can develop when toxins that the liver normally would filter are passed through the shunt directly into the bloodstream.
- TIPS is mainly used when all other treatments have failed or as a temporary measure in people awaiting a liver transplant.
- Placing pressure on varices to stop bleeding. If medication and endoscopy treatments don't work, doctors may try to stop bleeding by applying pressure to the esophageal varices. One way to temporarily stop bleeding is by inflating a balloon to put pressure on the varices for up to 24 hours, a procedure called balloon tamponade. Balloon tamponade is a temporary measure before other treatments can be performed, such as TIPS.
- This procedure carries a high risk of bleeding recurrence after the balloon is deflated. Balloon tamponade may also cause serious complications, including a rupture in the esophagus, which can lead to death.
- Restoring blood volume. You might be given a transfusion to replace lost blood and a clotting factor to stop bleeding.
- Preventing infection. There is an increased risk of infection with bleeding, so you'll likely be given an antibiotic to prevent infection.
- Replacing the diseased liver with a healthy one. Liver transplant is an option for people with severe liver disease or those who experience recurrent bleeding of esophageal varices. Although liver transplantation is often successful, the number of people awaiting transplants far outnumbers the available organs.
Re-bleeding
There is a high risk that bleeding will recur in people who've had bleeding from esophageal varices. Beta blockers and endoscopic band ligation are the recommended treatments to help prevent re-bleeding.
After initial banding treatment, your doctor will repeat your upper endoscopy at regular intervals and apply more bands if necessary until the esophageal varices are gone or small enough to reduce the risk of further bleeding.
Potential future treatment
Doctors are exploring an experimental emergency therapy to stop bleeding from esophageal varices that involves spraying an adhesive powder. The hemostatic powder is administered through a catheter during an endoscopy. When sprayed on the esophagus, hemostatic powder sticks to the varices and may stop bleeding.
Another potential way to stop bleeding when all other measures fail is to use self-expanding metal stents (SEMS). SEMS can be placed during an endoscopy and stop bleeding by placing pressure on the bleeding esophageal varices.
However, SEMS could damage tissue and can migrate after being placed. The stent should be removed within seven days and bleeding could recur. This option is experimental and isn't yet widely available.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Esophageal varices and Learn More about Diseases

Nightmare disorder
Ehlers-Danlos syndrome
Myocardial ischemia

Granuloma annulare

Bulimia nervosa

Hemorrhoids (Piles)
Schizophrenia
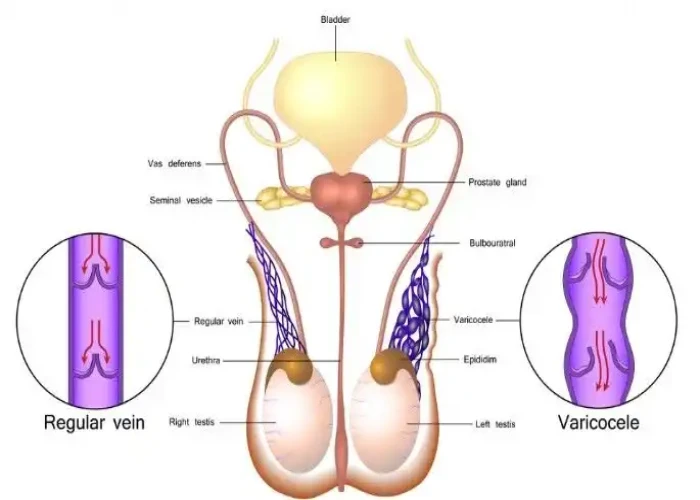
Varicocele
esophageal varices, ইসফাজিল ভ্যারিসেস
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.