Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
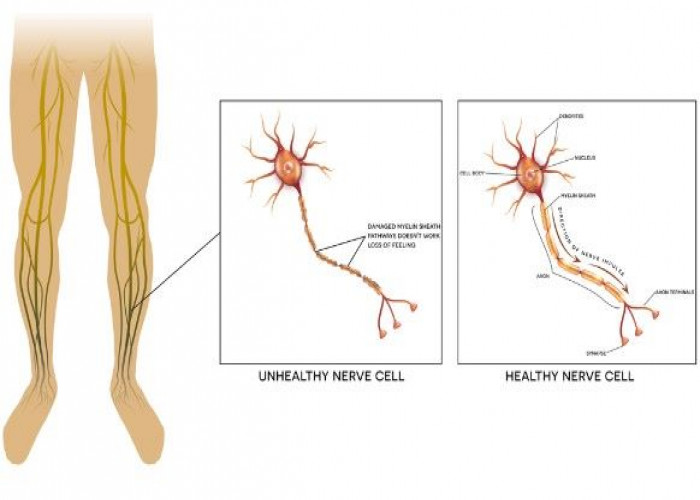
Diabetic neuropathy
Diabetic neuropathy is a type of nerve damage that occurs in people with diabetes. It can affect the nerves in various parts of the body, such as the feet, legs, hands, and arms. High blood sugar levels over time can cause damage to the nerves and lead to symptoms such as numbness, tingling, and pain.
There are several types of diabetic neuropathy, including peripheral neuropathy, autonomic neuropathy, proximal neuropathy, and focal neuropathy. Peripheral neuropathy is the most common type and affects the nerves that control sensation and movement in the limbs. Autonomic neuropathy affects the nerves that control internal organs such as the heart, bladder, and digestive system. Proximal neuropathy affects the nerves in the thighs, hips, and buttocks, and can cause weakness and pain. Focal neuropathy affects a specific nerve or group of nerves, and can cause sudden weakness or pain in one area of the body.
The symptoms of diabetic neuropathy can vary depending on the type and location of the affected nerves. Peripheral neuropathy can cause numbness, tingling, burning, or shooting pain in the feet and legs. Autonomic neuropathy can cause symptoms such as dizziness, nausea, vomiting, diarrhea, and bladder problems. Proximal neuropathy can cause severe pain in the thighs, hips, and buttocks, and can lead to weakness in the legs. Focal neuropathy can cause sudden weakness or pain in one area of the body.
Preventing diabetic neuropathy involves proper diabetes management, including regular monitoring of blood sugar levels and maintaining a healthy lifestyle. People with diabetes should also avoid smoking and excessive alcohol consumption. Treatment of diabetic neuropathy involves managing the symptoms and preventing further damage to the nerves. Medications such as pain relievers, antidepressants, and anticonvulsants may be prescribed to manage the symptoms. Physical therapy and exercise can also help improve muscle strength and reduce pain.
In conclusion, diabetic neuropathy is a common complication of diabetes that can cause nerve damage and lead to a range of symptoms. By managing your diabetes and taking steps to prevent complications, you can help protect your health and well-being. If you experience symptoms of diabetic neuropathy, it is important to seek medical attention to prevent further damage to the nerves.
Research Papers
Disease Signs and Symptoms
- Numbness
- High blood sugar
- Double vision (diplopia)
- Abdomen pain
- Groin pain or hip pain
- Reduced sexual desire
- Nausea or vomiting
- Loss of appetite
- Ulcer
- Joint pain
- Bone pain
- Cramp
- Skin pain or burning sensation
- Diabetes
Disease Causes
Diabetic neuropathy
The exact cause of each type of neuropathy is unknown. Researchers think that over time, uncontrolled high blood sugar damages nerves and interferes with their ability to send signals, leading to diabetic neuropathy. High blood sugar also weakens the walls of the small blood vessels (capillaries) that supply the nerves with oxygen and nutrients.
Disease Prevents
Diabetic neuropathy
You can prevent or delay diabetic neuropathy and its complications by closely managing your blood sugar and taking good care of your feet.
Blood sugar management
The American Diabetes Association recommends that people with diabetes have an A1C test at least twice a year. This test estimates your average blood sugar level for the past two to three months.
A1C goals may need to be individualized, but for many adults, the American Diabetes Association recommends an A1C of less than 7%. If your blood sugar levels are higher than your goal, you may need changes in your daily management, such as adding or adjusting your medications or changing your diet.
Foot care
Foot problems, including sores that don't heal, ulcers and even amputation, are common complications of diabetic neuropathy. But you can prevent many of these problems by having a thorough foot exam at least once a year, having your doctor check your feet at each office visit and taking good care of your feet at home.
Follow your doctor's recommendations for good foot care. To protect the health of your feet:
- Check your feet every day. Look for blisters, cuts, bruises, cracked and peeling skin, redness, and swelling. Use a mirror or ask a friend or family member to help examine parts of your feet that are hard to see.
- Keep your feet clean and dry. Wash your feet every day with lukewarm water and mild soap. Avoid soaking your feet. Dry your feet and between your toes carefully.
- Moisturize your feet. This helps prevent cracking. But don't get lotion between your toes, because it might encourage fungal growth.
- Trim your toenails carefully. Cut your toenails straight across. File the edges carefully to avoid sharp edges.
- Wear clean, dry socks. Look for socks made of cotton or moisture-wicking fibers that don't have tight bands or thick seams.
- Wear cushioned shoes that fit well. Always wear shoes or slippers to protect your feet. Make sure your shoes fit properly and allow your toes to move. A foot doctor can teach you how to buy properly fitted shoes and to prevent problems such as corns and calluses. If you qualify for Medicare, your plan may cover the cost of at least one pair of shoes each year.
Disease Treatments
Diabetic neuropathy has no known cure. The goals of treatment are to:
- Slow progression of the disease
- Relieve pain
- Manage complications and restore function
Slowing progression of the disease
Consistently keeping your blood sugar within your target range is the key to preventing or delaying nerve damage. Good blood sugar management may even improve some of your current symptoms. Your doctor will figure out the best target range for you based on factors including your age, how long you've had diabetes and your overall health.
Blood sugar levels may need to be individualized. But, in general, the American Diabetes Association recommends the following target blood sugar levels for most people with diabetes:
- Between 80 and 130 mg/dL, which is 4.4 and 7.2 millimoles per liter (mmol/L) before meals
- Less than 180 mg/dL (10.0 mmol/L) two hours after meals
Mayo Clinic encourages slightly lower blood sugar levels for most younger people with diabetes, and slightly higher levels for older people who may be more at risk of low blood sugar complications. Mayo Clinic generally recommends the following target blood sugar levels before meals:
- Between 80 and 120 mg/dL (4.4 and 6.7 mmol/L) for people age 59 and younger who have no other medical conditions
- Between 100 and 140 mg/dL (5.6 and 7.8 mmol/L) for people age 60 and older, or for those who have other medical conditions, including heart, lung or kidney disease
Other important ways to help slow or prevent neuropathy from getting worse include keeping your blood pressure under control, maintaining a healthy weight and getting regular physical activity.
Relieving pain
Many prescription medications are available for diabetes-related nerve pain, but they don't work for everyone. When considering any medication, talk to your doctor about the benefits and possible side effects to find what might work best for you.
Pain-relieving prescription treatments may include:
- Anti-seizure drugs. Some medications used to treat seizure disorders (epilepsy) are also used to ease nerve pain. The American Diabetes Association recommends starting with pregabalin (Lyrica). Gabapentin (Gralise, Neurontin) also is an option. Side effects may include drowsiness, dizziness and swelling.
- Antidepressants. Some antidepressants ease nerve pain, even if you aren't depressed. Tricyclic antidepressants may help with mild to moderate nerve pain. Drugs in this class include amitriptyline, desipramine (Norpramin) and imipramine (Tofranil). Side effects can be bothersome and include dry mouth and drowsiness.
- Serotonin and norepinephrine reuptake inhibitors (SNRIs) are another type of antidepressant that may help with nerve pain and have fewer side effects. The American Diabetes Association recommends duloxetine (Cymbalta) as a first treatment. Another that may be used is venlafaxine (Effexor XR). Possible side effects include nausea, sleepiness, dizziness, decreased appetite and constipation.
Sometimes, an antidepressant may be combined with an anti-seizure drug. These drugs can also be used with pain-relieving medication, such as an over-the-counter medication including acetaminophen (Tylenol, others) or ibuprofen (Advil, Motrin IB, others) or a skin patch with lidocaine (a numbing substance).
Managing complications and restoring function
To manage complications, you may need care from different specialists, such as a doctor that treats urinary tract problems (urologist) and a heart doctor (cardiologist), who can help prevent or treat complications.
The treatment you'll need depends on the neuropathy-related complication you have:
- Urinary tract problems. Some drugs affect bladder function, so your doctor may recommend stopping or changing medications. A strict urination schedule or urinating every few hours (timed urination) while applying gentle pressure to the bladder area (below your bellybutton) can help some bladder problems. Other methods, including self-catheterization, may be needed to remove urine from a nerve-damaged bladder.
- Digestive problems. To relieve mild signs and symptoms of gastroparesis — indigestion, belching, nausea or vomiting — doctors suggest eating smaller, more-frequent meals. Diet changes and medications may help relieve gastroparesis, diarrhea, constipation and nausea.
- Low blood pressure on standing (orthostatic hypotension). Treatment starts with simple lifestyle changes, such as avoiding alcohol, drinking plenty of water, and changing positions such as sitting or standing slowly. Sleeping with the head of the bed raised 6 to 10 inches helps prevent swings in blood pressure. Your doctor may also recommend compression support for your abdomen (abdominal binder). Several medications, either alone or together, may be used to treat orthostatic hypotension.
- Sexual dysfunction. Medications taken by mouth or injection may improve sexual function in some men, but they aren't safe and effective for everyone. Mechanical vacuum devices may increase blood flow to the penis. Women may find relief with vaginal lubricants.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Diabetic neuropathy and Learn More about Diseases

Common cold in babies

Vulvar cancer

Chiari malformation

Hyperhidrosis
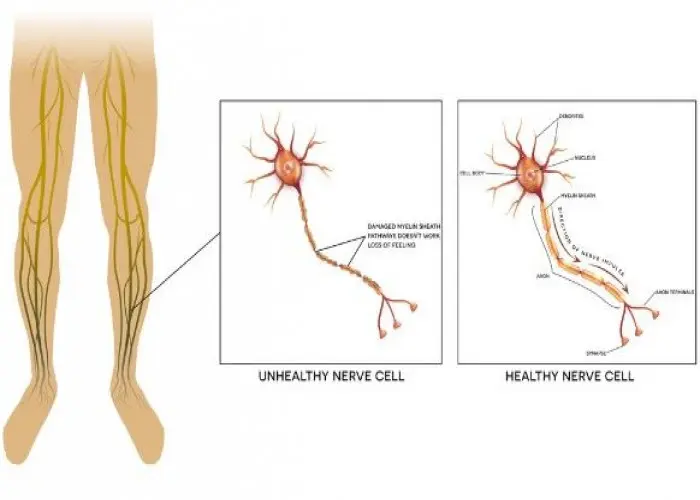
Spermatocele
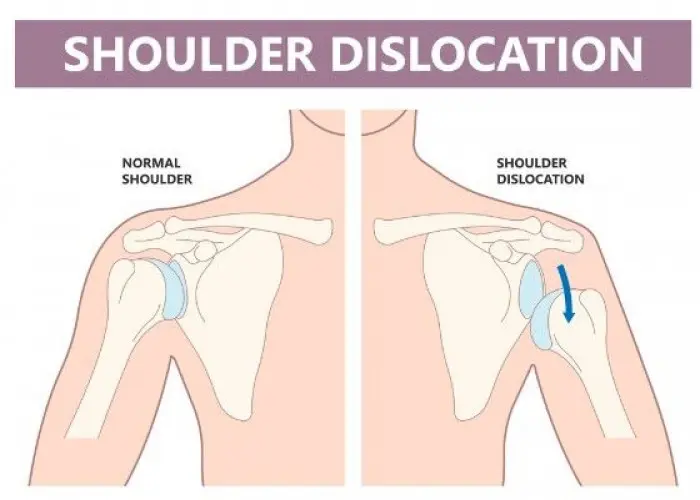
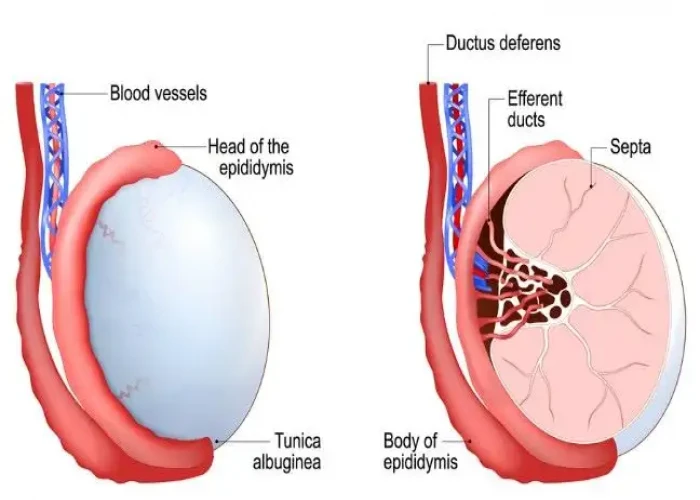
Dislocated shoulder
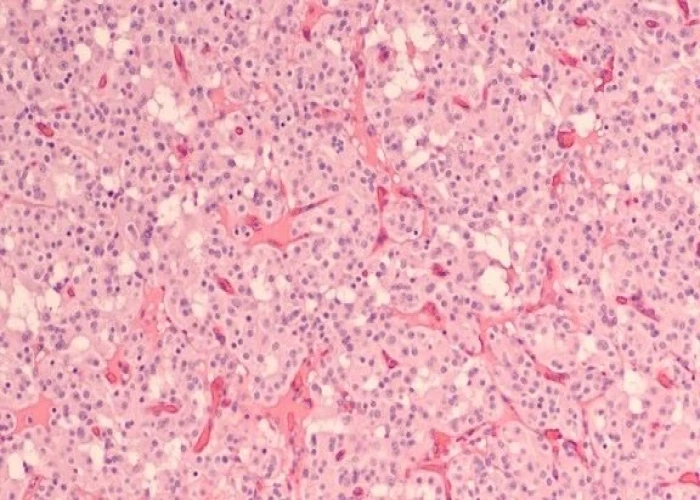
Pancreatic neuroendocrine tumors
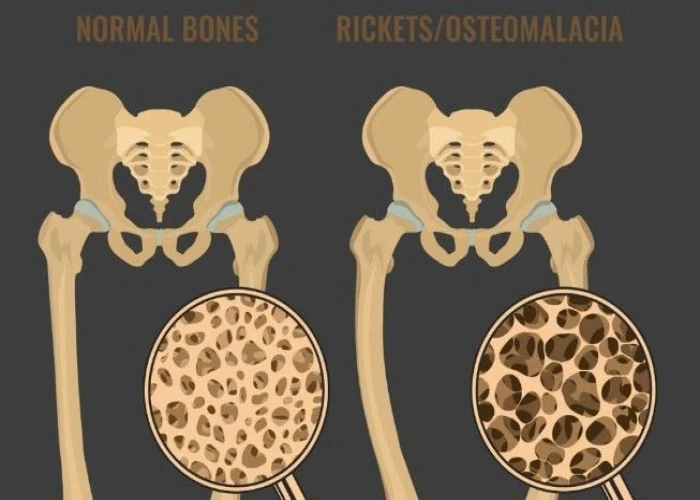
Osteomalacia
diabetic neuropathy, ডায়াবেটিক নিউরোপ্যাথি
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.