 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Intrapartum prophylaxis against group B streptococcal infections - Generics
Intrapartum prophylaxis against Group B Streptococcus (GBS) infections is a preventive measure used during labor and delivery to reduce the risk of GBS infection in newborns. GBS is a type of bacteria that is commonly found in the vagina and rectum of healthy women, and can be transmitted to the baby during delivery.
Intrapartum prophylaxis involves giving antibiotics to women who are at high risk of transmitting GBS to their newborns during delivery. The antibiotics are typically given intravenously, and the timing and duration of the prophylaxis depend on a number of factors, such as the woman's GBS status, gestational age, and the presence of risk factors such as premature rupture of membranes or a prolonged labor.
The use of intrapartum prophylaxis has been shown to significantly reduce the incidence of early-onset GBS disease, which can cause serious infections such as sepsis, pneumonia, and meningitis in newborns. However, it is important to note that intrapartum prophylaxis is not always 100% effective, and there is still a small risk of GBS infection in newborns even with prophylaxis.
To reduce the risk of GBS infection in newborns, pregnant women should be screened for GBS colonization between 35 and 37 weeks of gestation. Women who test positive for GBS colonization should receive intrapartum prophylaxis during labor and delivery, while those who test negative do not need prophylaxis unless they develop risk factors during labor. Women who have had a previous baby with GBS disease or who have other risk factors may also receive intrapartum prophylaxis even if they test negative for GBS colonization.
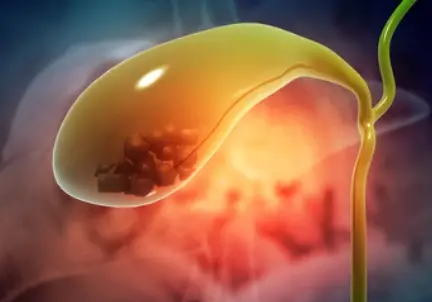
Chronic cholelithiasis

Polymyositis

Vincents infection

Cluster headache

Discomfort of the eye

Ocular hypertension
Insomnia
Germ cell tumors
Intrapartum prophylaxis against group B streptococcal infections, গ্রুপ বি স্ট্রেপ্টোকোকাল সংক্রমণের বিরুদ্ধে ইন্ট্রাপার্টাম প্রফিল্যাক্সিস
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.