 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Drug International Ltd.

Dorubin 20mg / 4ml
Generic for Diseases
- AIDS-related Kaposis sarcoma xx
- Acute Lymphocytic Leukemia
- Acute myeloid leukemia
- Hodgkins lymphoma
- Kaposis sarcoma
- Leukemia
Daunorubicin has antimitotic and cytotoxic activity through a number of proposed mechanisms of action. It forms complexes with DNA by intercalation between base pairs. It inhibits topoisomerase II activity by stabilizing the DNA- topoisomerase II complex, preventing the religation portion of the ligation- religation reaction that topoisomerase II catalyzes. Single strand and double-strand DNA breaks result. It may also inhibit polymerase activity, affect the regulation of gene expression, and produce free radical damage to DNA. It possesses an antitumor effect against a wide spectrum of animal tumors, either grafted or spontaneous.
Distribution: Daunorubicin is rapidly and widely distributed in tissues, with the highest levels in the spleen, kidneys, liver, lungs and heart. The drug binds to many cellular components, particularly nucleic acids. There is no evidence that it crosses the blood-brain barrier, but the drug apparently crosses the placenta.
Metabolism and Elimination: Daunorubicin is extensively metabolized in the liver and other tissues, mainly by cytoplasmic aldo-keto reductases, producing daunorubicinol, the major metabolite which has antineoplastic activity. Approximately 40% of the drug in the plasma is present as daunorubicinol within 30 minutes and 60% in 4 hours after a dose of Daunorubicin. Further metabolism via reduction cleavage of the glycosidic bond, 4-O demethylation, and conjugation with both sulfate and glucuronide have been demonstrated. Simple glycosidic cleavage of Daunorubicin or Daunorubicinol is not a significant metabolic pathway in man. Twenty-five percent of an administered dose of Daunorubicin is eliminated in an active form by urinary excretion and an estimated 40% by biliary excretion.
Daunorubicin in combination with other approved anticancer drugs is indicated for remission induction in acute nonlymphocytic leukemia (myelogenous, monocytic, erythroid) of adults and for remission induction in acute lymphocytic leukemia of children and adults.
Parenteral drug products should be inspected visually for particulate matter prior to administration.
Representative Dose Schedules and Combination for the Approved Indication of Remission Induction in Adult Acute Nonlymphocytic Leukemia: In Combination: For patients under age 60, Daunorubicin 45 mg/m2/day IV on days 1, 2, and 3 of the first course and on days 1, 2 of subsequent courses AND cytosine arabinoside 100 mg/m2/day IV infusion daily for 7 days for the first course and for 5 days for subsequent courses. For patients 60 years of age and above, Daunorubicin 30 mg/m2/day IV on days 1, 2, and 3 of the first course and on days 1, 2 of subsequent courses AND cytosine arabinoside 100 mg/m2/day IV infusion daily for 7 days for the first course and for 5 days for subsequent courses. This Daunorubicin dose-reduction is based on a single study and may not be appropriate if optimal supportive care is available.
Representative Dose Schedule and Combination for the Approved Indication of Remission Induction in Pediatric Acute Lymphocytic Leukemia: In Combination: Daunorubicin 25 mg/m2 IV on day 1 every week, Vincristine 1.5 mg/m2 IV on day 1 every week, prednisone 40 mg/m2 PO daily. Generally, a complete remission will be obtained within four such courses of therapy; however, if after four courses the patient is in partial remission, an additional one or, if necessary, two courses may be given in an effort to obtain a complete remission. In children less than 2 years of age or below 0.5 m2 body surface area, it has been recommended that the Daunorubicin dosage calculation should be based on weight (1 mg/kg) instead of body surface area.
Representative Dose Schedules and Combination for the Approved Indication of Remission Induction in Adult Acute Lymphocytic Leukemia: In Combination: Daunorubicin 45 mg/m2/day IV on days 1, 2, and 3 and Vincristine 2 mg IV on days 1, 8, and 15; prednisone 40 mg/m2/day PO on days 1 through 22, then tapered between days 22 to 29; L-asparaginase 500 IU/kg/day x 10 days IV on days 22 through 32. Or, as directed by the registered physicians.
It is contraindicated in patients with known hypersensitivity to Daunorubicin or any other components of this product.
Dose-limiting toxicity includes myelosuppression and cardiotoxicity. Other reactions include:
- Cutaneous: Reversible alopecia occurs in most patients. Rash, contact dermatitis and urticaria have occurred rarely.
- Gastrointestinal: Acute nausea and vomiting occur but are usually mild. Antiemetic therapy may be of some help. Mucositis may occur 3 to 7 days after administration. Diarrhea and abdominal pain have occasionally been reported.
- Local: If extravasation occurs during administration, severe local tissue necrosis, severe cellulitis, thrombophlebitis or painful induration can result.
- Acute Reactions: Rarely, anaphylactoid reaction, fever, and chills can occur. Hyperuricemia may occur, especially in patients with leukemia, and serum uric acid levels should be monitored.
Therapy with Daunorubicin requires close patient observation and frequent complete blood-count determinations. Cardiac, renal, and hepatic function should be evaluated prior to each course of treatment. Appropriate measures must be taken to control any systemic infection before beginning therapy with Daunorubicin. It may transiently impart a red coloration to the urine after administration, and patients should be advised to expect this.
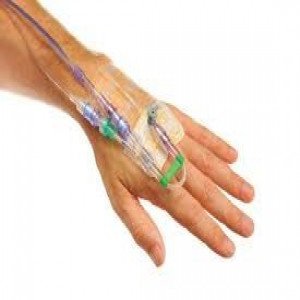
Daunorubicin Hydrochloride Injection must be given into a rapidly flowing intravenous infusion. It must never be given by the intramuscular or subcutaneous route. Severe local tissue necrosis will occur if there is extravasation during administration.
Myocardial toxicity manifested in its most severe form by potentially fatal congestive heart failure may occur either during therapy or months to years after termination of therapy. The incidence of myocardial toxicity increases after a total cumulative dose exceeding 400 to 550 mg/m2 in adults, 300 mg/m2 in children more than 2 years of age, or 10 mg/kg in children less than 2 years of age.
Severe myelosuppression occurs when used in therapeutic doses; this may lead to infection or hemorrhage.
It is recommended that Daunorubicin Hydrochloride be administered only by physicians who are experienced in leukemia chemotherapy and in facilities with laboratory and supportive resources adequate to monitor drug tolerance and protect and maintain a patient compromised by drug toxicity. The physician and institution must be capable of responding rapidly and completely to severe hemorrhagic conditions and/or overwhelming infection.
Dosage should be reduced in patients with impaired hepatic or renal function.
Pregnancy & Lactation
Pregnancy Category D. It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from Daunorubicin, mothers should be advised to discontinue nursing during Daunorubicin therapy.
Dorubin 20mg / 4ml and more Available Brands
Fungistat
Nifecap 10mg
Levoflox 750mg
Palnox 0.5mg
Cikolin 500mg
Cardinex 6000Anti-X...
Canasa 400mg
Depomed 2mg
...
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.