 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Shellfish allergy

Shellfish allergy is a type of food allergy that occurs when the immune system overreacts to proteins found in shellfish, such as shrimp, crab, lobster, and clams. It is one of the most common food allergies, affecting millions of people worldwide.
Symptoms of shellfish allergy can range from mild to severe and can include:
- Hives or skin rash
- Itching or tingling in the mouth
- Swelling of the lips, tongue, or throat
- Shortness of breath or wheezing
- Abdominal pain, nausea, or vomiting
- Diarrhea
- Dizziness or fainting
In severe cases, shellfish allergy can cause a life-threatening allergic reaction called anaphylaxis, which can cause difficulty breathing, rapid pulse, and a drop in blood pressure.
There is currently no cure for shellfish allergy, and the best way to manage it is to avoid eating shellfish and all foods that may contain shellfish or shellfish derivatives. People with shellfish allergy should also be cautious about cross-contamination, which can occur when shellfish comes into contact with other foods during preparation, cooking, or serving.
If you have shellfish allergy, it is important to carry an epinephrine auto-injector at all times and to seek immediate medical attention if you experience symptoms of anaphylaxis. An allergist can help diagnose and manage shellfish allergy, and may recommend medications such as antihistamines or corticosteroids to treat milder symptoms.
Research Papers
Disease Signs and Symptoms
- Hives
- Allergy
- Loss of consciousness (fainting)
- Dizziness, lightheadedness or faintness
- Dizziness (vertigo)
- Nausea or vomiting
- Diarrhea
- Abdomen pain
- Swollen lip
- Eczema
- Itching
- Shock with a severe drop in blood pressure
Disease Causes
Shellfish allergy
All food allergies are caused by an immune system overreaction. In shellfish allergy, your immune system mistakenly identifies a certain protein in shellfish as harmful, triggering the production of antibodies to the shellfish protein (allergen). The next time you come in contact with the allergen, your immune system releases histamine and other chemicals that cause allergy symptoms.
Types of shellfish
There are several types of shellfish, each containing different proteins:
- Crustaceans include crabs, lobster, crayfish, shrimp and prawn.
- Mollusks include squid, snails, clams, oysters and scallops.
Some people are allergic to only one type of shellfish but can eat others. Other people with shellfish allergy must avoid all shellfish.
Disease Prevents
Shellfish allergy
If you have a shellfish allergy, the only way to avoid an allergic reaction is to avoid all shellfish and products that contain shellfish. Even trace amounts of shellfish can cause a severe reaction in some people.
Avoiding shellfish
- Be cautious when dining out. When dining at restaurants, always check to make sure that the pan, oil or utensils used for shellfish aren't also used to prepare other foods, creating cross-contamination. It might be necessary to avoid eating at seafood restaurants, where there's a high risk of cross-contamination.
- Read labels. Cross-contamination can occur in stores where other food is processed or displayed near shellfish and during manufacturing. Read food labels carefully.
- Shellfish is rarely a hidden ingredient, but it may be in fish stock or seafood flavoring. Companies are required to label any product that contains shellfish or other foods that often cause allergic reactions, but the regulations don't apply to mollusks, such as clams, oysters and scallops.
- Keep your distance. You may need to completely avoid places where shellfish are prepared or processed. Some people react after touching shellfish or inhaling steam from cooking shellfish.
If you have a shellfish allergy, talk with your doctor about carrying emergency epinephrine. Consider wearing a medical alert bracelet or necklace that lets others know you have a food allergy.
One thing you don't need to worry about is if you'll also be allergic to iodine or radiocontrast dye that's used in some imaging tests. Even though shellfish contain small amounts of iodine, shellfish allergy is unrelated to the reactions some people have to radiocontrast material or iodine.
Disease Treatments
The only sure way to prevent an allergic reaction to shellfish is to avoid shellfish. But despite your best efforts, you may come into contact with shellfish.
Your doctor may instruct you to treat a mild allergic reaction to shellfish with medications such as antihistamines to reduce signs and symptoms, such as a rash and itchiness.
If you have a severe allergic reaction to shellfish (anaphylaxis), you'll likely need an emergency injection of epinephrine (adrenaline). If you're at risk of having a severe reaction, carry injectable epinephrine (EpiPen, Adrenaclick, others) with you at all times.
If you're at risk for anaphylaxis to shellfish, your doctor may instruct you to administer epinephrine even at the first sign of an allergic reaction. After you use epinephrine, seek emergency medical care, even if you've started to feel better.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Shellfish allergy and Learn More about Diseases

Voice disorders
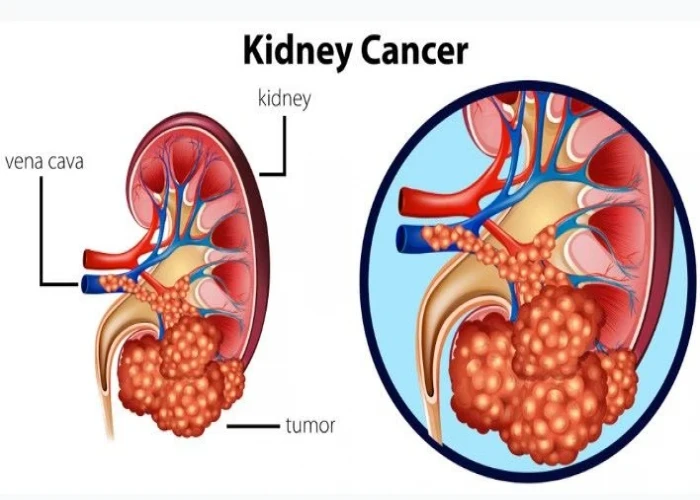
Kidney cancer

Foreign Body in eye
Shigella infection

Primary ovarian insufficiency

Wheat allergy

Psoriatic arthritis

Pruritus Vulva
shellfish allergy, শেলফিশ অ্যালার্জি
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
