 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Reactive arthritis

Reactive arthritis, also known as Reiter's syndrome, is a type of arthritis that occurs as a reaction to an infection, typically in the gastrointestinal or genitourinary tract. The condition is called reactive arthritis because it is a reaction to an infection in the body, rather than a direct result of the infection itself.
Symptoms of reactive arthritis can include joint pain, swelling, and stiffness, typically in the lower extremities, as well as inflammation in other parts of the body, such as the eyes or urinary tract. In addition, some people with reactive arthritis may develop skin rashes or mouth ulcers.
The underlying cause of reactive arthritis is not fully understood, but it is thought to be related to the body's immune response to the infection. The condition is typically diagnosed based on a physical exam, medical history, and blood tests, and sometimes imaging studies.
Treatment for reactive arthritis may include nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce pain and inflammation, as well as physical therapy or other forms of exercise to improve joint function. In more severe cases, disease-modifying antirheumatic drugs (DMARDs) or biological medications may be used to help slow the progression of the condition.
Prevention of reactive arthritis involves taking steps to prevent infections that can trigger the condition, such as practicing safe sex and avoiding contaminated food and water. If you experience symptoms of reactive arthritis, it is important to seek medical attention right away to determine the appropriate treatment plan.
Research Papers
Disease Signs and Symptoms
- Eye pain or burning
- Inflammation of soft tissue where it enters bone (enthesitis).
- Increased frequency and discomfort during urination may occur, as can inflammation of the prostate gland or cervix.
- Joint stiffness
- Swollen feet and ankles (edema)
- Swollen knee
- Knee pain
- Sprained joint
- Joint pain
- Swollen eye (Conjunctivitis)
- Low back pain
- The joint pain associated with reactive arthritis most commonly occurs in the knees, ankles and feet.
- This might include muscles, tendons and ligaments.
Disease Causes
Reactive arthritis
Reactive arthritis develops in reaction to an infection in your body, often in your intestines, genitals or urinary tract. You might not be aware of the triggering infection if it causes mild symptoms or none at all.
Numerous bacteria can cause reactive arthritis. Some are transmitted sexually, and others are foodborne. The most common ones include:
- Campylobacter
- Chlamydia
- Clostridioides difficile
- Escherichia coli
- Salmonella
- Shigella
- Yersinia
Reactive arthritis isn't contagious. However, the bacteria that cause it can be transmitted sexually or in contaminated food. Only a few of the people who are exposed to these bacteria develop reactive arthritis.
Disease Prevents
Reactive arthritis
Genetic factors appear to play a role in whether you're likely to develop reactive arthritis. Though you can't change your genetic makeup, you can reduce your exposure to the bacteria that may lead to reactive arthritis.
Store your food at proper temperatures and cook it properly. Doing these things help you avoid the many foodborne bacteria that can cause reactive arthritis, including salmonella, shigella, yersinia and campylobacter. Some sexually transmitted infections can trigger reactive arthritis. Use condoms to help lower your risk.
Disease Treatments
The goal of treatment is to manage your symptoms and treat an infection that could still be present.
Medications
If your reactive arthritis was triggered by a bacterial infection, your doctor might prescribe an antibiotic if there is evidence of persistent infection. Which antibiotic you take depends on the bacteria that are present.
Signs and symptoms of reactive arthritis may be eased with:
- Nonsteroidal anti-inflammatory drugs (NSAIDs). Prescription NSAIDs, such as indomethacin (Indocin), can relieve the inflammation and pain of reactive arthritis.
- Steroids. A steroid injection into affected joints can reduce inflammation and allow you to return to your usual activity level. Steroid eye drops may be used for eye symptoms, and steroid creams might be used for skin rashes.
- Rheumatoid arthritis drugs. Limited evidence suggests that medications such as sulfasalazine (Azulfidine), methotrexate (Trexall) or etanercept (Enbrel) can relieve pain and stiffness for some people with reactive arthritis.
Physical therapy
A physical therapist can provide you with targeted exercises for your joints and muscles. Strengthening exercises increase the joint's support by developing the muscles around the affected joints. Range-of-motion exercises can increase your joints' flexibility and reduce stiffness.
Disease Diagnoses
Disease Allopathic Generics
-
Aspirin
Pills should be powdered and mixed with water.
First 1 pill 3 times a day after meals. Then 2 pills 3 times a day.
-
Paracetamol
1 pill 3 times a day.
-
Indomethacin (Oral)
Aspirin and paracetamol do not reduce the pain.
1 capsule 3 times a day after meals.
-
Ibuprofen
1 tablet of 400 mg 3 times a day.
-
Ketoprofen (Oral & injection)
1 capsule 1/2 time a day 1 to 2 hours before or 2 hours after meals, between meals or after meals.
-
Celecoxib
1+0+1 or 0+0+200mg after meals.
-
Mefenamic acid
Elderly patients 500 mg 1 tablet 2/3 times a day after or between meals. Cannot be used for more than 7 days.
-
Naproxen Sodium
Medicines containing naproxen can be used in rheumatoid arthritis.
Adult 500mg 1 time between or after meals 2 times a day.
-
Ketorolac Tromethamine
1+0+1 or 1+1+1.
-
Tramadol Hydrochloride
1+0+1 or 1+1+1 (10/15 days).
-
Tolperisone Hydrochloride
1+0+1
-
Leflunomide
100 mg daily for 3 days.
-
Prednisolone
1 pill 3 times a day for 5/7 days.
-
Dexamethasone
1 pill 3 times a day for 5/7 days.
-
Betamethasone
First increase and then decrease gradually.
-
Ranitidine Hydrochloride
150 mg pill 2 times a day.
-
Famotidine
1 pill of 20/40mg in the morning and 1 pill at night.
- Diclofenac Sodium
-
Fluoxetine Hydrochloride
1 pill every morning after breakfast for 1 month.
-
Nortriptyline
Take 1 pill at night before going to bed.
-
Vitamin B complex
Take 1 pill daily after food.
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Reactive arthritis and Learn More about Diseases

Bunions

Hyperhidrosis

Male hypogonadism

Priapism

Pericarditis
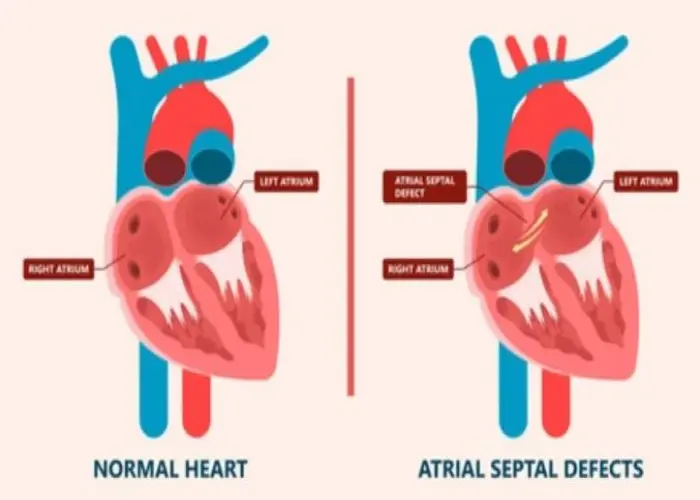
Atrial septal defect (ASD)

Gonorrhea

Keratoconus
reactive arthritis, প্রতিক্রিয়াশীল বাত
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
