 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
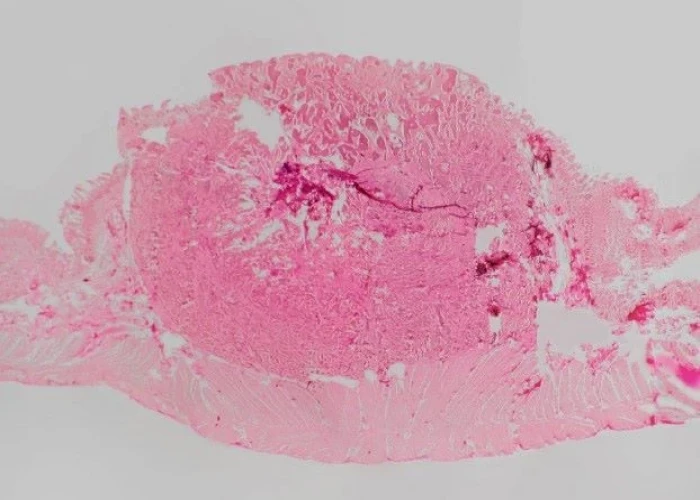
Preeclampsia

Preeclampsia is a pregnancy complication that typically occurs after 20 weeks of gestation and is characterized by high blood pressure and damage to organs, most commonly the liver and kidneys. Preeclampsia can also affect the placenta, which can lead to fetal growth restriction and other complications.
The exact cause of preeclampsia is not known, but it is thought to be related to problems with the development of blood vessels in the placenta. Risk factors for preeclampsia include first-time pregnancy, multiple pregnancies, a history of high blood pressure or kidney disease, and obesity.
Symptoms of preeclampsia may include high blood pressure, protein in the urine, swelling of the hands and feet, headaches, blurred vision, and abdominal pain. If left untreated, preeclampsia can lead to serious complications such as seizures, stroke, and organ failure.
The treatment for preeclampsia typically involves close monitoring of the mother and the fetus, and may include medications to control blood pressure and prevent seizures. In some cases, delivery of the baby may be necessary to prevent further complications. If preeclampsia is detected early and managed appropriately, most women and their babies recover without serious complications.
Regular prenatal care and monitoring by a healthcare provider is important for the early detection and management of preeclampsia. Women who are at high risk of developing preeclampsia may need additional monitoring and interventions during pregnancy to prevent complications.
Research Papers
Disease Signs and Symptoms
- Excess protein or cloudy urine (proteinuria)
- Excess protein in the urine (proteinuria) or additional signs of kidney problems
- Swollen (Edema)
- Rapid weight gain
- Shortness of breath (dyspnea)
- Decreased levels of platelets in the blood (thrombocytopenia)
- Nausea or vomiting
- Abdomen pain
- Sensitivity to light (Photophobia)
- Blurred vision of eye
- Headaches
- Shortness of breath, caused by fluid in lungs
Disease Causes
Preeclampsia
The exact cause of preeclampsia involves several factors. Experts believe it begins in the placenta — the organ that nourishes the fetus throughout pregnancy. Early in pregnancy, new blood vessels develop and evolve to efficiently send blood to the placenta.
In women with preeclampsia, these blood vessels don't seem to develop or function properly. They're narrower than normal blood vessels and react differently to hormonal signaling, which limits the amount of blood that can flow through them.
Causes of this abnormal development may include:
- Insufficient blood flow to the uterus
- Damage to the blood vessels
- A problem with the immune system
- Certain genes
Other high blood pressure disorders during pregnancy
Preeclampsia is classified as one of four high blood pressure disorders that can occur during pregnancy. The other three are:
- Gestational hypertension. Women with gestational hypertension have high blood pressure but no excess protein in their urine or other signs of organ damage. Some women with gestational hypertension eventually develop preeclampsia.
- Chronic hypertension. Chronic hypertension is high blood pressure that was present before pregnancy or that occurs before 20 weeks of pregnancy. But because high blood pressure usually doesn't have symptoms, it may be hard to determine when it began.
- Chronic hypertension with superimposed preeclampsia. This condition occurs in women who have been diagnosed with chronic high blood pressure before pregnancy, but then develop worsening high blood pressure and protein in the urine or other health complications during pregnancy.
Disease Prevents
Preeclampsia
Researchers continue to study ways to prevent preeclampsia, but so far, no clear strategies have emerged. Eating less salt, changing your activities, restricting calories, or consuming garlic or fish oil doesn't reduce your risk. Increasing your intake of vitamins C and E hasn't been shown to have a benefit.
Some studies have reported an association between vitamin D deficiency and an increased risk of preeclampsia. But while some studies have shown an association between taking vitamin D supplements and a lower risk of preeclampsia, others have failed to make the connection.
In certain cases, however, you may be able to reduce your risk of preeclampsia with:
- Low-dose aspirin. If you meet certain risk factors — including a history of preeclampsia, a multiple pregnancy, chronic high blood pressure, kidney disease, diabetes or autoimmune disease — your doctor may recommend a daily low-dose aspirin (81 milligrams) beginning after 12 weeks of pregnancy.
- Calcium supplements. In some populations, women who have calcium deficiency before pregnancy — and who don't get enough calcium during pregnancy through their diets — might benefit from calcium supplements to prevent preeclampsia. However, it's unlikely that women from the United States or other developed countries would have calcium deficiency to the degree that calcium supplements would benefit them.
It's important that you don't take any medications, vitamins or supplements without first talking to your doctor.
Before you become pregnant, especially if you've had preeclampsia before, it's a good idea to be as healthy as you can be. Lose weight if you need to, and make sure other conditions, such as diabetes, are well-managed.
Once you're pregnant, take care of yourself — and your baby — through early and regular prenatal care. If preeclampsia is detected early, you and your doctor can work together to prevent complications and make the best choices for you and your baby.
Disease Treatments
The most effective treatment for preeclampsia is delivery. You're at increased risk of seizures, placental abruption, stroke and possibly severe bleeding until your blood pressure decreases. Of course, if it's too early in your pregnancy, delivery may not be the best thing for your baby.
If you're diagnosed with preeclampsia, your doctor will let you know how often you'll need to come in for prenatal visits — likely more frequently than what's typically recommended for pregnancy. You'll also need more frequent blood tests, ultrasounds and nonstress tests than would be expected in an uncomplicated pregnancy.
Medications
Possible treatment for preeclampsia may include:
- Medications to lower blood pressure. These medications, called antihypertensives, are used to lower your blood pressure if it's dangerously high. Blood pressure in the 140/90 millimeters of mercury (mm Hg) range generally isn't treated.
- Although there are many different types of antihypertensive medications, a number of them aren't safe to use during pregnancy. Discuss with your doctor whether you need to use an antihypertensive medicine in your situation to control your blood pressure.
- Corticosteroids. If you have severe preeclampsia or HELLP syndrome, corticosteroid medications can temporarily improve liver and platelet function to help prolong your pregnancy. Corticosteroids can also help your baby's lungs become more mature in as little as 48 hours — an important step in preparing a premature baby for life outside the womb.
- Anticonvulsant medications. If your preeclampsia is severe, your doctor may prescribe an anticonvulsant medication, such as magnesium sulfate, to prevent a first seizure.
Bed rest
Bed rest used to be routinely recommended for women with preeclampsia. But research hasn't shown a benefit from this practice, and it can increase your risk of blood clots, as well as impact your economic and social lives. For most women, bed rest is no longer recommended.
Hospitalization
Severe preeclampsia may require that you be hospitalized. In the hospital, your doctor may perform regular nonstress tests or biophysical profiles to monitor your baby's well-being and measure the volume of amniotic fluid. A lack of amniotic fluid is a sign of poor blood supply to the baby.
Delivery
If you're diagnosed with preeclampsia near the end of your pregnancy, your doctor may recommend inducing labor right away. The readiness of your cervix — whether it's beginning to open (dilate), thin (efface) and soften (ripen) — also may be a factor in determining whether or when labor will be induced.
In severe cases, it may not be possible to consider your baby's gestational age or the readiness of your cervix. If it's not possible to wait, your doctor may induce labor or schedule a C-section right away. During delivery, you may be given magnesium sulfate intravenously to prevent seizures.
If you need pain-relieving medication after your delivery, ask your doctor what you should take. NSAIDs, such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve), can increase your blood pressure.
After delivery, it can take some time before high blood pressure and other preeclampsia symptoms resolve.
Disease Diagnoses
Disease Allopathic Generics
-
Ampicillin Sodium
Medicines containing ampicillin to relieve urinary tract infections.
1 each 4 times a day 5/7 days.
-
Amoxicillin Trihydrate
1 every 4 times a day 5/7 days.
-
Cephalexin
1 every 6 times a day 5/7 days.
-
Ciprofloxacin
1 pill in the morning 1 pill at night 7-14 days.
-
Cefuroxime Axetil
1+0+1 (7 days).
-
Vitamin B complex
1 capsule 2 times a day after meals.
-
Ferrous Fumarate
1 pill 2/3 times a day after meals.
-
Zinc Sulfate Monohydrate
1 daily.
-
Folic Acid
1 pill 3 times a day after meals.
-
Multivitamin & Multimineral
1 pill 1 times a day after meals.
-
Calcium Carbonate
1 will run daily.
-
Frusemide (Furosemide)
40/20mg 1 time a day or 1 day after 3/4 days.
-
Diazepam
1 injection into the flesh.
-
Pethidine Hydrochloride
An injection should be given in the flesh.
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Preeclampsia and Learn More about Diseases
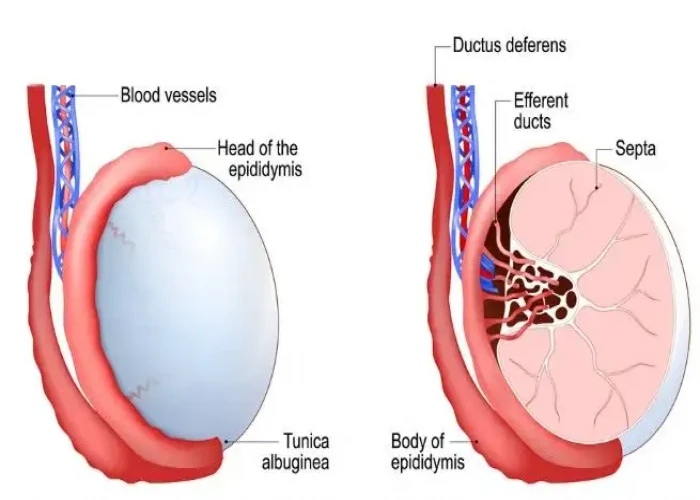
Scrotal masses

Tularemia
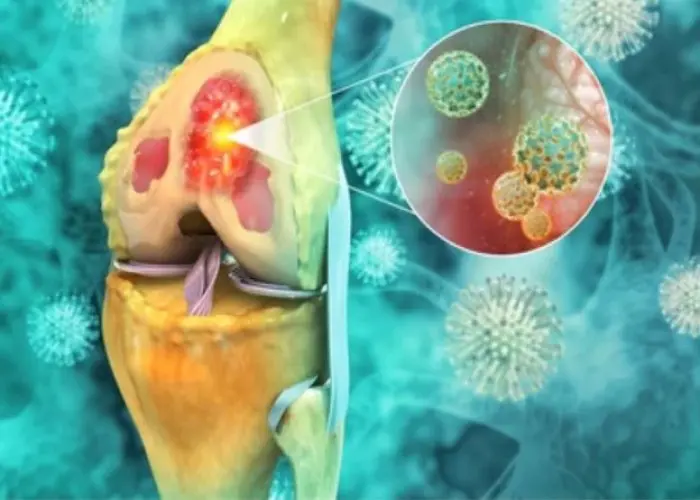
Bone cancer
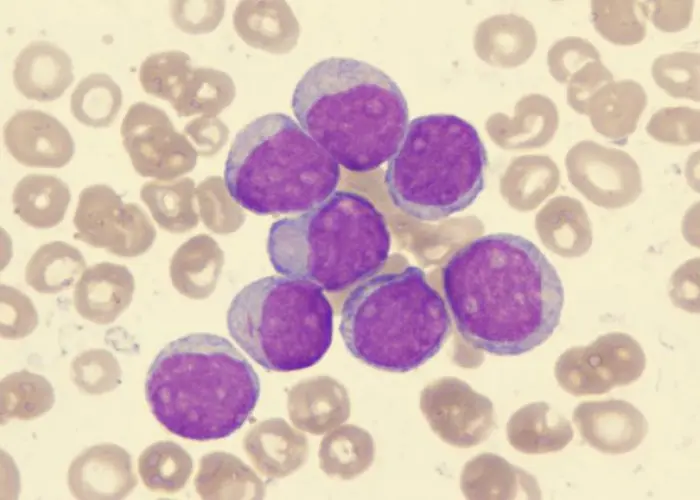
Acute myelogenous leukemia
Atypical depression

Roseola

Illness anxiety disorder
Neuroendocrine tumors
preeclampsia, প্রিক্ল্যাম্পসিয়া
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
