 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Postpartum depression

Postpartum depression (PPD) is a type of depression that occurs after childbirth. It is a common condition that affects up to 1 in 7 women who give birth. PPD can develop within the first few weeks after childbirth, but it can also occur up to a year after giving birth.
Symptoms of PPD may include feelings of sadness, anxiety, irritability, or hopelessness, changes in appetite or sleep patterns, loss of interest in activities, difficulty bonding with the baby, and thoughts of self-harm or suicide.
Risk factors for PPD may include a personal or family history of depression, a difficult pregnancy or childbirth, a lack of social support, or experiencing other stressful life events around the time of childbirth.
Treatment for PPD may involve a combination of medication, psychotherapy, and lifestyle changes. Antidepressant medication may be used to help manage symptoms, while psychotherapy, such as cognitive-behavioral therapy (CBT), can help women develop coping skills and strategies to manage negative thoughts and feelings. Lifestyle changes, such as getting regular exercise, eating a healthy diet, and getting adequate sleep, can also help improve symptoms.
It is important to seek medical attention if symptoms of PPD are present, as early diagnosis and treatment can help improve outcomes and minimize complications. Women who experience symptoms of PPD should talk to their healthcare provider or a mental health professional to discuss treatment options and develop a plan for managing their symptoms.
Research Papers
Disease Signs and Symptoms
- Anxiety
- Obsessive thoughts about your baby
- Frequent or recurrent thoughts of death
- Thoughts of harming yourself baby
- Feelings of worthlessness, shame, guilt or inadequacy
- Reduced interest and pleasure in activities you used to enjoy
- Withdrawing from family and friends
- Difficulty bonding with baby
- Rapid mood chang
- Trouble sleep (insomnia)
- Memory loss
- Frequent crying
- Irritability
- High blood pressure (hypertension) — 140/90 millimeters of mercury (mm Hg) or greater
Disease Causes
Postpartum depression
There's no single cause of postpartum depression, but physical and emotional issues may play a role.
- Physical changes. After childbirth, a dramatic drop in hormones (estrogen and progesterone) in your body may contribute to postpartum depression. Other hormones produced by your thyroid gland also may drop sharply — which can leave you feeling tired, sluggish and depressed.
- Emotional issues. When you're sleep deprived and overwhelmed, you may have trouble handling even minor problems. You may be anxious about your ability to care for a newborn. You may feel less attractive, struggle with your sense of identity or feel that you've lost control over your life. Any of these issues can contribute to postpartum depression.
Disease Prevents
Postpartum depression
If you have a history of depression — especially postpartum depression — tell your doctor if you're planning on becoming pregnant or as soon as you find out you're pregnant.
- During pregnancy, your doctor can monitor you closely for signs and symptoms of depression. He or she may have you complete a depression-screening questionnaire during your pregnancy and after delivery. Sometimes mild depression can be managed with support groups, counseling or other therapies. In other cases, antidepressants may be recommended — even during pregnancy.
- After your baby is born, your doctor may recommend an early postpartum checkup to screen for signs and symptoms of postpartum depression. The earlier it's detected, the earlier treatment can begin. If you have a history of postpartum depression, your doctor may recommend antidepressant treatment or psychotherapy immediately after delivery.
Disease Treatments
Treatment and recovery time vary, depending on the severity of your depression and your individual needs. If you have an underactive thyroid or an underlying illness, your doctor may treat those conditions or refer you to the appropriate specialist. Your doctor may also refer you to a mental health professional.
Baby blues
The baby blues usually fade on their own within a few days to one to two weeks. In the meantime:
- Get as much rest as you can.
- Accept help from family and friends.
- Connect with other new moms.
- Create time to take care of yourself.
- Avoid alcohol and recreational drugs, which can make mood swings worse.
Postpartum depression
Postpartum depression is often treated with psychotherapy (also called talk therapy or mental health counseling), medication or both.
- Psychotherapy. It may help to talk through your concerns with a psychiatrist, psychologist or other mental health professional. Through therapy, you can find better ways to cope with your feelings, solve problems, set realistic goals and respond to situations in a positive way. Sometimes family or relationship therapy also helps.
- Antidepressants. Your doctor may recommend an antidepressant. If you're breast-feeding, any medication you take will enter your breast milk. However, most antidepressants can be used during breast-feeding with little risk of side effects for your baby. Work with your doctor to weigh the potential risks and benefits of specific antidepressants.
With appropriate treatment, postpartum depression symptoms usually improve. In some cases, postpartum depression can continue, becoming chronic depression. It's important to continue treatment after you begin to feel better. Stopping treatment too early may lead to a relapse.
Postpartum psychosis
Postpartum psychosis requires immediate treatment, usually in the hospital. Treatment may include:
- Medication. Treatment may require a combination of medications — such as antipsychotic medications, mood stabilizers and benzodiazepines — to control your signs and symptoms.
- Electroconvulsive therapy (ECT). If your postpartum depression is severe and you experience postpartum psychosis, ECT may be recommended if symptoms do not respond to medication. ECT is a procedure in which small electrical currents are passed through the brain, intentionally triggering a brief seizure. ECT seems to cause changes in brain chemistry that can reduce the symptoms of psychosis and depression, especially when other treatments have been unsuccessful.
Treatment for postpartum psychosis can challenge a mother's ability to breast-feed. Separation from the baby makes breast-feeding difficult, and some medications used to treat postpartum psychosis aren't recommended for women who are breast-feeding. If you're experiencing postpartum psychosis, your doctor can help you work through these challenges.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Postpartum depression and Learn More about Diseases

Convergence insufficiency

Peptic ulcer
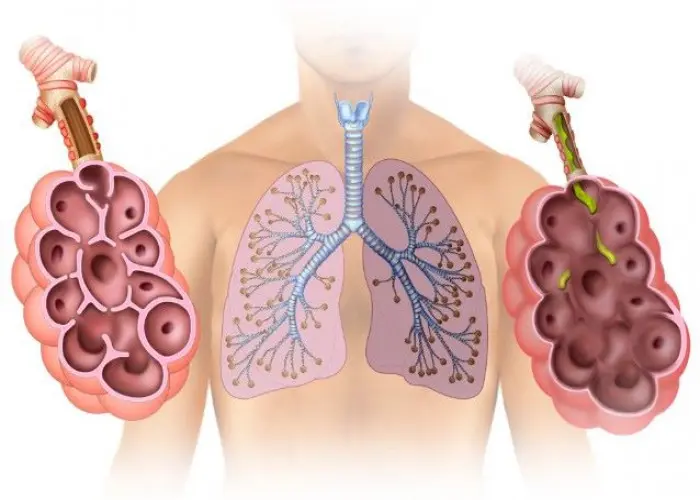
Emphysema

Cryoglobulinemia

Tularemia
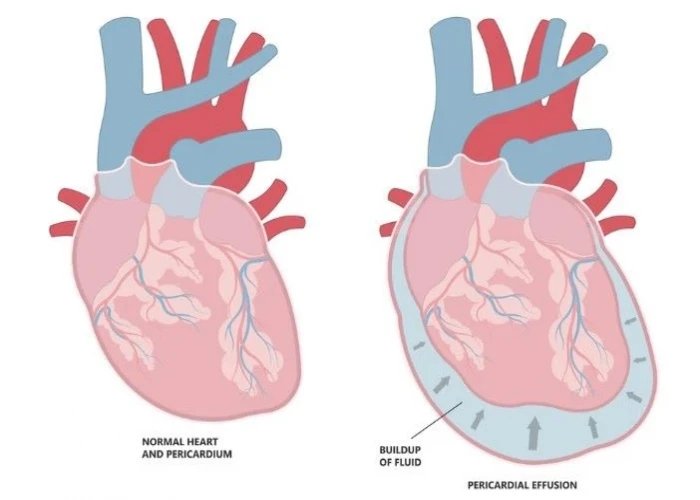
Pericardial effusion

Stress fractures

Eosinophilic esophagitis
postpartum depression, প্রসবের বিষণ্নতা
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
