Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Pheochromocytoma
Pheochromocytoma is a rare tumor that develops in the adrenal glands, which are located above the kidneys. These tumors are usually benign (non-cancerous), but can sometimes be malignant (cancerous) and spread to other parts of the body.
Pheochromocytoma tumors can cause the adrenal gland to produce excessive amounts of hormones called catecholamines, which can cause a variety of symptoms. These symptoms can include high blood pressure, headache, sweating, rapid heartbeat, anxiety, and palpitations. Pheochromocytoma can also cause episodes of severe hypertension, which can be life-threatening if not treated promptly.
The exact cause of pheochromocytoma is not known, but it is thought to be related to genetic mutations that cause the cells of the adrenal gland to grow and divide abnormally. Risk factors for pheochromocytoma include certain genetic disorders, such as multiple endocrine neoplasia type 2 (MEN 2) and von Hippel-Lindau disease.
The main treatment for pheochromocytoma is the surgical removal of the tumor. Before surgery, medications may be given to help control blood pressure and prevent episodes of hypertension. After surgery, individuals may need to be monitored for a period of time to ensure that the tumor has been completely removed and that blood pressure has returned to normal.
In some cases, pheochromocytoma may be associated with other tumors in the body, such as paragangliomas. Therefore, a thorough evaluation and follow-up may be necessary to monitor for the development of other tumors.
Research Papers
Disease Signs and Symptoms
- High blood pressure (hypertension)
- Headaches
- Heavy sweating (diaphoresis)
- Rapid heartbeat (tachycardia)
- Tremors or muscle jerking
- Shortness of breath (dyspnea)
- Anxiety
- Constipation
- Weight loss
Disease Causes
Pheochromocytoma
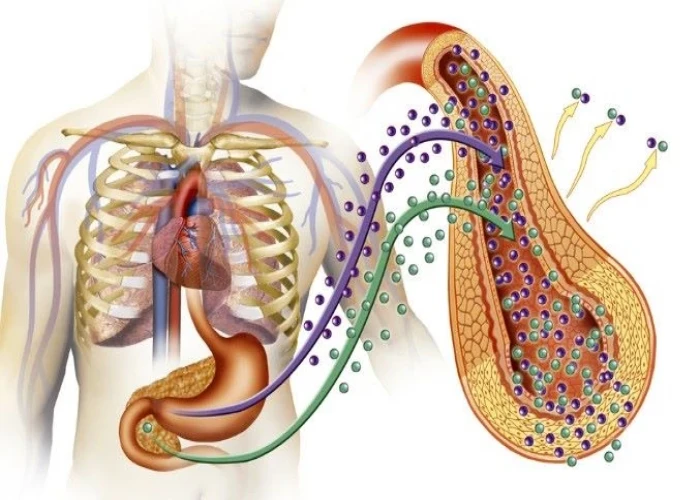
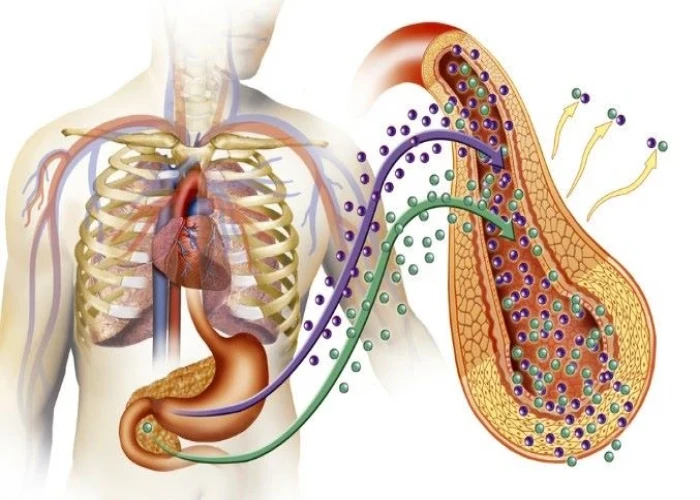
Researchers don't know exactly what causes a pheochromocytoma. The tumor develops in specialized cells, called chromaffin cells, located in the center of an adrenal gland. These cells release certain hormones, primarily adrenaline (epinephrine) and noradrenaline (norepinephrine), that help control many body functions, such as heart rate, blood pressure and blood sugar.
The role of hormones
Adrenaline and noradrenaline trigger your body's fight-or-flight response to a perceived threat. The hormones cause your blood pressure to increase and your heart to beat faster. They prepare other body systems that enable you to react quickly. A pheochromocytoma causes more of these hormones to be released and causes them to be released when you're not in a threatening situation.
Related tumors
While most of the chromaffin cells are located in the adrenal glands, small clusters of these cells are also in the heart, head, neck, bladder, back wall of the abdomen and along the spine. Chromaffin cell tumors, called paragangliomas, may result in the same effects on the body.
Disease Prevents
Disease Treatments
The primary treatment for a pheochromocytoma is surgery to remove the tumor. Before you have surgery, your doctor will likely prescribe specific blood pressure medications that block the actions of the high-adrenaline hormones to lower the risk of developing dangerously high blood pressure during surgery.
Preoperative preparations
You'll likely take two drugs for seven to 10 days that help lower blood pressure before surgery. These drugs will either replace or be added to other blood pressure drugs you take.
- Alpha blockers. These drugs keep smaller arteries and veins open and relaxed, improving blood flow and decreasing blood pressure. Alpha blockers include phenoxybenzamine, doxazosin (Cardura) and prazosin (Minipress). Side effects might include irregular heartbeat, dizziness, fatigue, vision problems, sexual dysfunction in men and swelling in the limbs.
- Beta blockers. These drugs cause your heart to beat more slowly and with less force. They also help keep blood vessels open and relaxed. In your surgery preparation, your doctor will likely prescribe a beta blocker several days after starting the alpha blocker.
- Beta blockers include atenolol (Tenormin), metoprolol (Lopressor, Toprol-XL) and propranolol (Inderal, Innopran XL). Possible side effects include fatigue, upset stomach, headache, dizziness, constipation, diarrhea, irregular heartbeat, difficulty breathing and swelling in the limbs.
- High-salt diet. Alpha and beta blockers widen the blood vessels, causing the amount of fluid within the blood vessels to be low. This can cause dangerous drops in blood pressure with standing. A high-salt diet will draw more fluid inside the blood vessels, preventing the development of low blood pressure during and after surgery.
Surgery
In most cases, your surgeon removes the entire adrenal gland with a pheochromocytoma with minimally invasive surgery. Your surgeon will make a few small openings through which he or she inserts wandlike devices equipped with video cameras and small tools.
The remaining healthy adrenal gland carries out the functions normally performed by two. Blood pressure usually returns to normal.
In some cases, such as when the other adrenal gland has been removed, your doctor might remove only the tumor, sparing some healthy tissue.
If a tumor is cancerous, the tumor and other cancerous tissue will be removed. However, even if all of the cancerous tissue isn't removed, surgery might limit hormone production and provide some blood pressure control.
Cancer treatments
Very few pheochromocytomas are cancerous. As such, research about the best treatments is limited. Treatments for cancerous tumors and cancer that has spread in the body, related to a pheochromocytoma, include:
- MIBG. This radiation therapy combines MIBG, a compound that attaches to adrenal tumors, with a type of radioactive iodine. The treatment goal is to deliver radiation therapy to a specific site and kill cancerous cells.
- Peptide receptor radionuclide therapy (PRRT). PRRT combines a drug that targets cancer cells with a small amount of a radioactive substance. It allows radiation to be delivered directly to the cancer cells. One PRRT drug, lutetium Lu 177 dotatate (Lutathera), is used to treat advanced neuroendocrine tumors.
- Chemotherapy. Chemotherapy is the use of powerful drugs that kill fast-growing cancer cells.
- Radiation therapy. This may be used for symptomatic treatment of tumors that have spread to the bone, for example, that are causing pain.
- Targeted cancer therapies. These medications hinder the function of naturally occurring molecules that promote the growth and spread of cancerous cells.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Pheochromocytoma and Learn More about Diseases

Cushing syndrome

Toxoplasmosis
Schizophrenia

Gingivitis
Hypopituitarism

Radiation enteritis

Urinary tract infection (UTI)

Genital herpes
pheochromocytoma, ফিওক্রোমোসাইটোমা
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.