 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Periodontitis (Pyrrhoea)

Periodontitis, also known as pyorrhea, is a serious gum infection that damages the soft tissue and destroys the bone that supports the teeth. It is a common type of periodontal disease and is typically caused by poor oral hygiene, but can also be influenced by genetic and environmental factors.
Periodontitis typically begins with inflammation of the gums, which is known as gingivitis. If left untreated, the inflammation can spread below the gumline and cause the formation of pockets between the gums and teeth. Bacteria and plaque can accumulate in these pockets, leading to further damage and eventual tooth loss.
Symptoms of periodontitis may include:
- Red, swollen, or tender gums
- Bleeding gums, especially when brushing or flossing
- Receding gums, which can make the teeth appear longer
- Loose or shifting teeth
- Painful chewing
- Persistent bad breath
Diagnosis of periodontitis usually involves a comprehensive dental exam, including X-rays, and may involve measuring the depth of the pockets between the teeth and gums. Treatment typically involves a combination of professional dental cleaning and at-home oral care. This may include:
- Scaling and root planing (deep cleaning below the gumline to remove plaque and tartar)
- Antibiotics to treat bacterial infection
- Surgery to remove infected tissue and/or bone grafts to regenerate lost bone
- Maintenance therapy to prevent the recurrence of periodontitis
Prevention of periodontitis involves maintaining good oral hygiene habits, such as brushing and flossing regularly, using mouthwash, and seeing a dentist for regular cleanings and checkups. It is also important to avoid tobacco use and to maintain a healthy diet.
Research Papers
Disease Signs and Symptoms
- Swollen gums
- Dark red gums
- Bleeding from gums
- Bad breath (halitosis)
- Loose teeth
- Pink-tinged toothbrush after brushing
- New spaces developing between teeth
- Gums that pull away from teeth (recede), making teeth look longer than normal
- A change in the way teeth fit together when biting
Disease Causes
Periodontitis
In most cases, the development of periodontitis starts with plaque — a sticky film composed mainly of bacteria. If left untreated, here's how plaque can eventually advance to periodontitis:
- Plaque forms on your teeth when starches and sugars in food interact with bacteria normally found in your mouth. Brushing your teeth twice a day and flossing once a day removes plaque, but plaque re-forms quickly.
- Plaque can harden under your gumline into tartar (calculus) if it stays on your teeth. Tartar is more difficult to remove and it's filled with bacteria. The longer plaque and tartar remain on your teeth, the more damage they can do. You can't get rid of tartar by brushing and flossing — you need a professional dental cleaning to remove it.
- Plaque can cause gingivitis, the mildest form of gum disease. Gingivitis is irritation and inflammation of the part of your gum tissue around the base of your teeth (gingiva). Gingivitis can be reversed with professional treatment and good home oral care.
- Ongoing gum inflammation can cause periodontitis, eventually causing pockets to develop between your gums and teeth that fill with plaque, tartar and bacteria. In time, these pockets become deeper, filling with more bacteria. If not treated, these deep infections cause a loss of tissue and bone, and ultimately you may lose one or more teeth. Also, ongoing chronic inflammation can put a strain on your immune system.
Disease Prevents
Periodontitis
The best way to prevent periodontitis is to follow a program of good oral hygiene, one that you begin early and practice consistently throughout life.
- Good oral hygiene. That means brushing your teeth for two minutes at least twice daily — in the morning and before going to bed — and flossing at least once a day. Flossing before you brush allows you to clean away the loosened food particles and bacteria. Good oral hygiene prevents the development of an environment around your teeth that is favorable to specific bacteria that cause periodontal disease.
- Regular dental visits. See your dentist or dental hygienist regularly for cleanings, usually every six to 12 months. If you have risk factors that increase your chance of developing periodontitis — such as having dry mouth, taking certain medications or smoking — you may need professional cleaning more often.
Disease Treatments
Treatment may be performed by a periodontist, a dentist or a dental hygienist. The goal of periodontitis treatment is to thoroughly clean the pockets around teeth and prevent damage to surrounding bone. You have the best chance for successful treatment when you also adopt a daily routine of good oral care, manage health conditions that may impact dental health and stop tobacco use.
Nonsurgical treatments
If periodontitis isn't advanced, treatment may involve less invasive procedures, including:
- Scaling. Scaling removes tartar and bacteria from your tooth surfaces and beneath your gums. It may be performed using instruments, a laser or an ultrasonic device.
- Root planing. Root planing smooths the root surfaces, discouraging further buildup of tartar and bacteria, and removes bacterial byproducts that contribute to inflammation and delay healing or reattachment of the gum to the tooth surfaces.
- Antibiotics. Topical or oral antibiotics can help control bacterial infection. Topical antibiotics can include antibiotic mouth rinses or insertion of gels containing antibiotics in the space between your teeth and gums or into pockets after deep cleaning. However, oral antibiotics may be necessary to completely eliminate infection-causing bacteria.
Surgical treatments
If you have advanced periodontitis, treatment may require dental surgery, such as:
- Flap surgery (pocket reduction surgery). Your periodontist makes tiny incisions in your gum so that a section of gum tissue can be lifted back, exposing the roots for more effective scaling and root planing. Because periodontitis often causes bone loss, the underlying bone may be recontoured before the gum tissue is sutured back in place. After you heal, it's easier to clean these areas and maintain healthy gum tissue.
- Soft tissue grafts. When you lose gum tissue, your gumline recedes. You may need to have some of the damaged soft tissue reinforced. This is usually done by removing a small amount of tissue from the roof of your mouth (palate) or using tissue from another donor source and attaching it to the affected site. This can help reduce further gum recession, cover exposed roots and give your teeth a more pleasing appearance.
- Bone grafting. This procedure is performed when periodontitis has destroyed the bone surrounding your tooth root. The graft may be composed of small fragments of your own bone, or the bone may be synthetic or donated. The bone graft helps prevent tooth loss by holding your tooth in place. It also serves as a platform for the regrowth of natural bone.
- Guided tissue regeneration. This allows the regrowth of bone that was destroyed by bacteria. In one approach, your dentist places a special piece of biocompatible fabric between existing bone and your tooth. The material prevents unwanted tissue from entering the healing area, allowing bone to grow back instead.
- Tissue-stimulating proteins. Another technique involves applying a special gel to a diseased tooth root. This gel contains the same proteins found in developing tooth enamel and stimulates the growth of healthy bone and tissue.
Disease Diagnoses
Disease Allopathic Generics
-
Benzydamine Hydrochloride
Medicines containing benzydamine hydrochloride for toothache.
1 after meals 3 times a day.
-
Ibuprofen
400mg 1 in the morning and 1 at night with or after food.
Ulcer and asthma patients should not eat.
-
Naproxen Sodium
1 pill 2 times a day after meals on a full stomach. 2+0+1
-
Aceclofenac
1+0+1 after meal
-
Ranitidine Hydrochloride
Medicines containing ranitidine to prevent gas.
1 pill in the morning after food 1 pill after thinking at night (1+0+1)
-
Omeprazole
Medicines containing ranitidine to prevent gas.
1 pill in the morning after food 1 pill after thinking at night (1+0+1)
-
Calcium Lactate
1 pill 2 times a day.
-
Calcium Carbonate
2 pills daily at noon or night.
-
Vitamin C [Ascorbic acid]
1 pill should be sucked 3 times a day. (1+1+1)
-
Amoxicillin Trihydrate
1 (250) pill 3 times a day for 7 days. If inflammation is high, 1 (500) (1+0+1).
-
Cephalexin
Adults take 1 capsule (250mg) 4 times a day at night. 5-12 years 250mg 3 times a day. Or adult (500mg) capsule 1+0+1 or 1+1+1
-
Metronidazole
Medicines containing metronidazole in case of pus at the root of the tooth.
1+1+1
-
Povidone Iodine
Povidone-iodine compound for mouth disinfection.
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Periodontitis (Pyrrhoea) and Learn More about Diseases
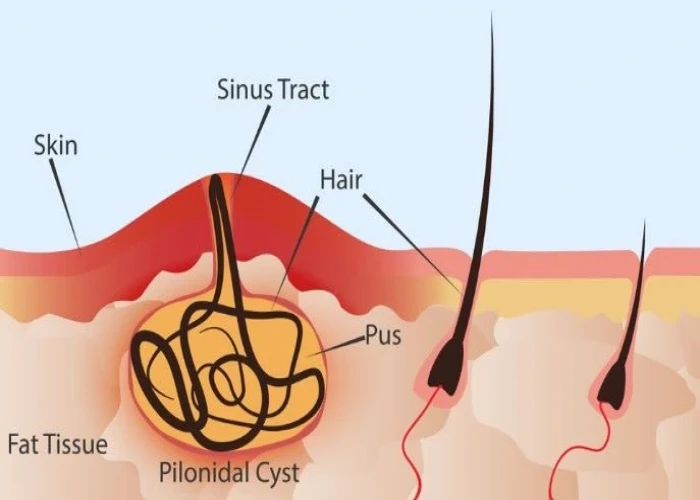
Pilonidal cyst

Frontal lobe seizures
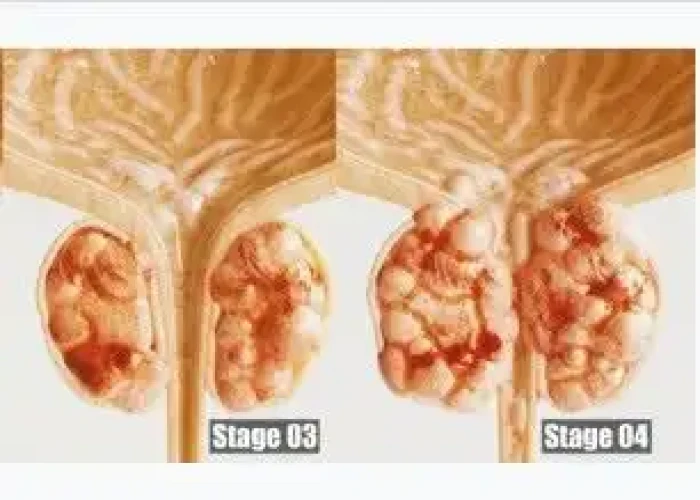
Stage 4 prostate cancer

Common warts
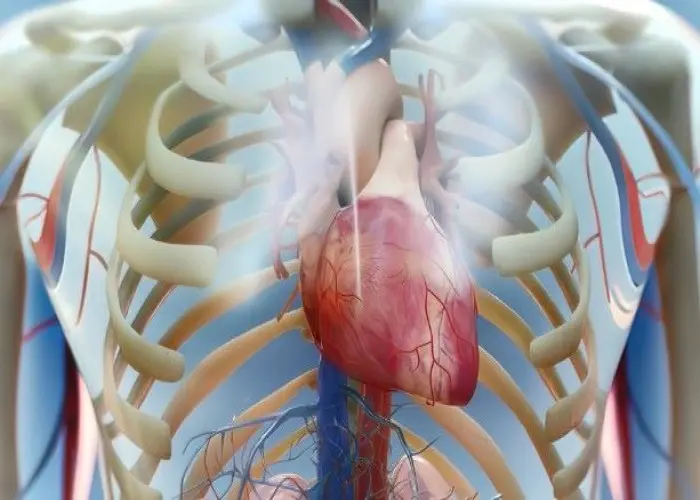
Cardiac Failure

Alzheimers disease

Central nervous system vascular malformations

Wheat allergy
Periodontitis, pyrrhoea, পিরিওডোনটাইটিস, দাঁতের প্রদাহ
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
