 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Obstructive sleep apnea
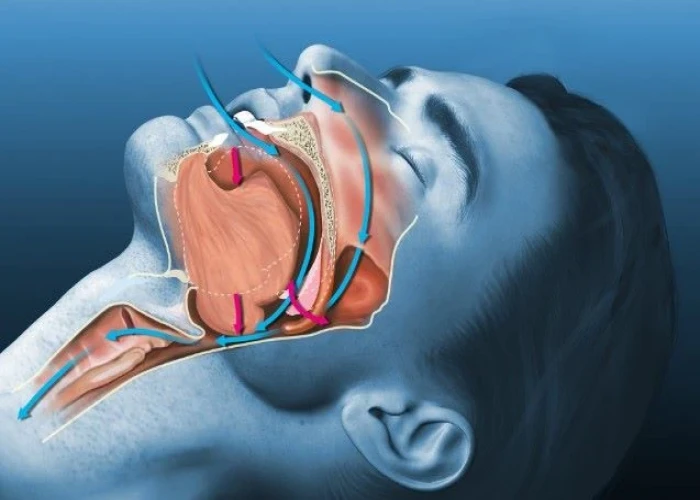
Obstructive sleep apnea (OSA) is a common sleep disorder in which a person's breathing is repeatedly interrupted during sleep. This occurs when the muscles at the back of the throat fail to keep the airway open, leading to pauses in breathing (apneas) or shallow breaths. These pauses in breathing can occur multiple times per hour, disrupting normal sleep patterns and leading to daytime sleepiness and other health problems.
Risk factors for OSA include obesity, a narrow airway, a family history of sleep apnea, and certain medical conditions such as diabetes and high blood pressure. Symptoms of OSA include loud snoring, pauses in breathing during sleep, gasping or choking during sleep, daytime sleepiness, and difficulty concentrating.
Diagnosis of OSA involves a sleep study, which may be conducted at a sleep center or using a home sleep test. Treatment for OSA typically involves lifestyle changes, such as weight loss and avoiding alcohol and sedatives before bedtime, as well as continuous positive airway pressure (CPAP) therapy. CPAP therapy involves wearing a mask over the nose or mouth that delivers pressurized air to keep the airway open during sleep. Other treatments may include oral appliances that reposition the jaw and tongue or surgery to remove excess tissue from the throat.
Untreated OSA can lead to a number of health problems, including high blood pressure, heart disease, stroke, and type 2 diabetes. It can also lead to accidents and decreased quality of life due to daytime sleepiness and fatigue. With appropriate treatment, however, most people with OSA are able to manage their symptoms and improve their quality of life.
Research Papers
Disease Signs and Symptoms
- Excessive daytime sleepiness
- High blood pressure (hypertension)
- Rapid mood chang
- Morning headaches
- Headaches
- Sore throat
- Dry mouth
- Stopped breathing during sleep
- Loud snoring (Noisy breathing)
- Abrupt awakenings accompanied by gasping or choking
Disease Causes
Obstructive sleep apnea
Obstructive sleep apnea occurs when the muscles in the back of your throat relax too much to allow normal breathing. These muscles support structures including the back of the roof of your mouth (soft palate), the triangular piece of tissue hanging from the soft palate (uvula), the tonsils and the tongue.
When the muscles relax, your airway narrows or closes as you breathe in, hampering your breathing for 10 seconds or longer. This can lower the level of oxygen in your blood and cause a buildup of carbon dioxide.
Your brain senses this impaired breathing and briefly rouses you from sleep so that you can reopen your airway. This awakening is usually so brief that you don't remember it.
You can awaken with shortness of breath that corrects itself quickly, within one or two deep breaths. You might make a snorting, choking or gasping sound.
This pattern can repeat itself five to 30 times or more each hour, all night long. These disruptions impair your ability to reach the deep, restful phases of sleep, and you'll probably feel sleepy during your waking hours.
People with obstructive sleep apnea might not be aware of their interrupted sleep. Many people with this type of sleep apnea don't realize they haven't slept well all night.
Disease Prevents
Disease Treatments
Lifestyle changes
For milder cases of obstructive sleep apnea, your doctor might recommend lifestyle changes:
- Lose weight if you're overweight.
- Exercise regularly.
- Drink alcohol moderately, if at all. Don't drink in the hours before bedtime.
- Quit smoking.
- Use a nasal decongestant or allergy medications.
- Don't sleep on your back.
- Avoid taking sedative medications such as anti-anxiety drugs or sleeping pills.
If these measures don't improve your sleep or if your apnea is moderate to severe, then your doctor may recommend other treatments. Certain devices can help open up a blocked airway. In other cases, surgery may be necessary.
Therapies
- Positive airway pressure. If you have obstructive sleep apnea, you may benefit from positive airway pressure. In this treatment, a machine delivers air pressure through a piece that fits into your nose or is placed over your nose and mouth while you sleep.
- Positive airway pressure reduces the number of respiratory events that occur as you sleep, reduces daytime sleepiness and improves your quality of life.
- The most common type is called continuous positive airway pressure, or CPAP (SEE-pap). With this treatment, the pressure of the air breathed is continuous, constant and somewhat greater than that of the surrounding air, which is just enough to keep your upper airway passages open. This air pressure prevents obstructive sleep apnea and snoring.
- Although CPAP is the most consistently successful and most commonly used method of treating obstructive sleep apnea, some people find the mask cumbersome, uncomfortable or loud. However, newer machines are smaller and less noisy than older machines and there are a variety of mask designs for individual comfort.
- Also, with some practice, most people learn to adjust the mask to obtain a comfortable and secure fit. You may need to try different types to find a suitable mask. Several options are available, such as nasal masks, nasal pillows or face masks.
- If you're having particular difficulties tolerating pressure, some machines have special adaptive pressure functions to improve comfort. You might also benefit from using a humidifier along with your CPAP system.
- CPAP may be given at a continuous (fixed) pressure or varied (autotitrating) pressure (APAP). In fixed CPAP, the pressure stays constant. In autotitrating CPAP, the levels of pressure are adjusted if the device senses increased airway resistance.
- Bilevel positive airway pressure (BPAP), another type of positive airway pressure, delivers a preset amount of pressure when you breathe in and a different amount of pressure when you breathe out.
- CPAP is more commonly used because it's been well studied for obstructive sleep apnea and has been shown to effectively treat obstructive sleep apnea. However, for people who have difficulty tolerating fixed CPAP, BPAP or APAP might be worth a try.
- Don't stop using your positive airway pressure machine if you have problems. Check with your doctor to see what adjustments you can make to improve its comfort.
- In addition, contact your doctor if you still snore despite treatment, if you begin snoring again, or if your weight goes up or down by 10% or more.
- Mouthpiece (oral device). Though positive airway pressure is often an effective treatment, oral appliances are an alternative for some people with mild or moderate obstructive sleep apnea. It's also used for people with severe sleep apnea who can't use CPAP. These devices may reduce your sleepiness and improve your quality of life.
- These devices are designed to keep your throat open. Some devices keep your airway open by bringing your lower jaw forward, which can sometimes relieve snoring and obstructive sleep apnea. Other devices hold your tongue in a different position.
- If you and your doctor decide to explore this option, you'll need to see a dentist experienced in dental sleep medicine appliances for the fitting and follow-up therapy. A number of devices are available. Close follow-up is needed to ensure successful treatment and that use of the device doesn't cause changes to your teeth.
Nasal masks
The mask covering the nose supplies air pressure.
Might be good if:
- Your doctor has prescribed a high air pressure setting
- You move around a lot in your sleep
Surgery or other procedures
Surgery is usually considered only if other therapies haven't been effective or haven't been appropriate options for you. Surgical options may include:
- Surgical removal of tissue. Uvulopalatopharyngoplasty (UPPP) is a procedure in which your doctor removes tissue from the back of your mouth and top of your throat. Your tonsils and adenoids may be removed as well. UPPP usually is performed in a hospital and requires a general anesthetic.
- Upper airway stimulation. This new device is approved for use in people with moderate to severe obstructive sleep apnea who can't tolerate CPAP or BPAP.
- A small, thin impulse generator (hypoglossal nerve stimulator) is implanted under the skin in the upper chest. The device detects your breathing patterns and, when necessary, stimulates the nerve that controls movement of the tongue.
- Studies have found that upper airway stimulation leads to significant improvement in obstructive sleep apnea symptoms and improvements in quality of life.
- Jaw surgery (maxillomandibular advancement). In this procedure, the upper and lower parts of your jaw are moved forward from the rest of your facial bones. This enlarges the space behind the tongue and soft palate, making obstruction less likely.
- Surgical opening in the neck (tracheostomy). You may need this form of surgery if other treatments have failed and you have severe, life-threatening obstructive sleep apnea.
- During a tracheostomy, your surgeon makes an opening in your neck and inserts a metal or plastic tube through which you breathe. Air passes in and out of your lungs, bypassing the blocked air passage in your throat.
Other types of surgery may help reduce snoring and sleep apnea by clearing or enlarging air passages, including:
- Nasal surgery to remove polyps or straighten a crooked partition between your nostrils (deviated septum)
- Surgery to remove enlarged tonsils or adenoids
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Obstructive sleep apnea and Learn More about Diseases

Transposition of the great arteries

Mosquito bites

Castleman disease
Absence seizure

Pregnancy Abodominal Pain
Buerger's disease
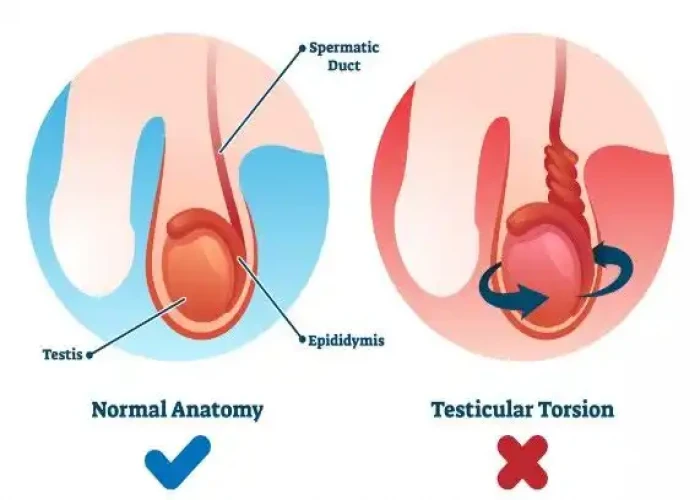
Testicular torsion

Amenorrhea
obstructive sleep apnea, অবস্ট্রাকটিভ স্লিপ অ্যাপনিয়া
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
