 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Miscarriage (Abortion)

Miscarriage, also known as spontaneous abortion, is the loss of a pregnancy before the 20th week. Miscarriage is a common occurrence, with up to 25% of pregnancies ending in miscarriage, often before the woman even realizes she is pregnant.
Miscarriage can be caused by a variety of factors, including chromosomal abnormalities, hormonal imbalances, infections, and structural problems with the uterus or cervix. Risk factors for miscarriage may include advanced maternal age, a history of previous miscarriages, smoking, alcohol or drug use, and certain medical conditions, such as diabetes or thyroid disorders.
Symptoms of miscarriage may include vaginal bleeding, cramping, and the passing of tissue or clots. However, not all women who experience these symptoms will have a miscarriage, as some bleeding and cramping can be normal during early pregnancy. A healthcare provider can perform an ultrasound and other tests to determine if a miscarriage has occurred.
Treatment for miscarriage may depend on the stage of pregnancy and the woman's individual situation. In some cases, the body will naturally expel the pregnancy tissue, and no further treatment is necessary. However, in other cases, a healthcare provider may recommend a procedure, such as a dilation and curettage (D&C) or medication, to help remove the remaining tissue and prevent infection.
Miscarriage can be a difficult and emotional experience for women and their partners. Supportive care and counseling may be helpful for coping with the physical and emotional aspects of a miscarriage. It is also important to receive appropriate medical care and follow-up to ensure that the miscarriage is complete and to address any underlying medical conditions that may have contributed to the loss.
Research Papers
Disease Signs and Symptoms
- Vaginal bleeding
- Abdomen pain
- Abdomen cramps
- Watery vaginal discharge
- Lower back pain
Disease Causes
Miscarriage
Problems with the genes or chromosomes
Most miscarriages occur because the fetus isn't developing as expected. About 50 percent of miscarriages are associated with extra or missing chromosomes. Most often, chromosome problems result from errors that occur by chance as the embryo divides and grows — not problems inherited from the parents.
Chromosome problems might lead to:
- Blighted ovum. Blighted ovum occurs when no embryo forms.
- Intrauterine fetal demise. In this situation, an embryo forms but stops developing and dies before any symptoms of pregnancy loss occur.
- Molar pregnancy and partial molar pregnancy. With a molar pregnancy, both sets of chromosomes come from the father. A molar pregnancy is associated with abnormal growth of the placenta; there is usually no fetal development.
- A partial molar pregnancy occurs when the mother's chromosomes remain, but the father provides two sets of chromosomes. A partial molar pregnancy is usually associated with abnormalities of the placenta, and an abnormal fetus.
- Molar and partial molar pregnancies are not viable pregnancies. Molar and partial molar pregnancies can sometimes be associated with cancerous changes of the placenta.
Maternal health conditions
In a few cases, a mother's health condition might lead to miscarriage. Examples include:
- Uncontrolled diabetes
- Infections
- Hormonal problems
- Uterus or cervix problems
- Thyroid disease
What does NOT cause miscarriage
Routine activities such as these don't provoke a miscarriage:
- Exercise, including high-intensity activities such as jogging and cycling.
- Sexual intercourse.
- Working, provided you're not exposed to harmful chemicals or radiation. Talk with your doctor if you are concerned about work-related risks.
Disease Prevents
Miscarriage
Often, there's nothing you can do to prevent a miscarriage. Simply focus on taking good care of yourself and your baby:
- Seek regular prenatal care.
- Avoid known miscarriage risk factors — such as smoking, drinking alcohol and illicit drug use.
- Take a daily multivitamin.
- Limit your caffeine intake. A recent study found that drinking more than two caffeinated beverages a day appeared to be associated with a higher risk of miscarriage.
If you have a chronic condition, work with your health care team to keep it under control.
Disease Treatments
Threatened miscarriage
For a threatened miscarriage, your health care provider might recommend resting until the bleeding or pain subsides. Bed rest hasn't been proved to prevent miscarriage, but it's sometimes prescribed as a safeguard. You might be asked to avoid exercise and sex, too. Although these steps haven't been proved to reduce the risk of miscarriage, they might improve your comfort.
In some cases, it's also a good idea to postpone traveling — especially to areas where it would be difficult to receive prompt medical care. Ask your health care provider if it would be wise to delay any upcoming trips you've planned.
Miscarriage
With ultrasound, it's now much easier to determine whether an embryo has died or was never formed. Either finding means that a miscarriage will definitely occur. In this situation, you might have several choices:
- Expectant management. If you have no signs of infection, you might choose to let the miscarriage progress naturally. Usually this happens within a couple of weeks of determining that the embryo has died. Unfortunately, it might take up to three or four weeks. This can be an emotionally difficult time. If expulsion doesn't happen on its own, medical or surgical treatment will be needed.
- Medical treatment. If, after a diagnosis of certain pregnancy loss, you'd prefer to speed the process, medication can cause your body to expel the pregnancy tissue and placenta. The medication can be taken by mouth or by insertion in the vagina. Your health care provider might recommend inserting the medication vaginally to increase its effectiveness and minimize side effects such as nausea and diarrhea. For about 70 to 90 percent of women, this treatment works within 24 hours.
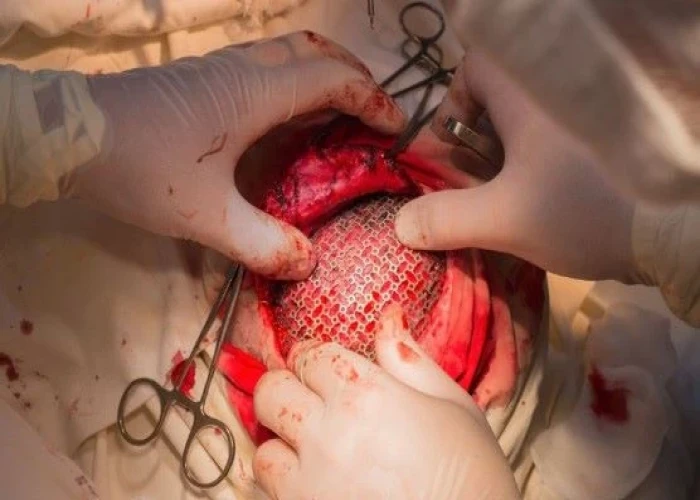
- Surgical treatment. Another option is a minor surgical procedure called suction dilation and curettage (D&C). During this procedure, your health care provider dilates your cervix and removes tissue from the inside of your uterus. Complications are rare, but they might include damage to the connective tissue of your cervix or the uterine wall. Surgical treatment is needed if you have a miscarriage accompanied by heavy bleeding or signs of an infection.
Physical recovery
In most cases, physical recovery from miscarriage takes only a few hours to a couple of days. In the meantime, call your health care provider if you experience heavy bleeding, fever or abdominal pain.
You may ovulate as soon as two weeks after a miscarriage. Expect your period to return within four to six weeks. You can start using any type of contraception immediately after a miscarriage. However, avoid having sex or putting anything in your vagina — such as a tampon — for two weeks after a miscarriage.
Future pregnancies
It's possible to become pregnant during the menstrual cycle immediately after a miscarriage. But if you and your partner decide to attempt another pregnancy, make sure you're physically and emotionally ready. Ask your health care provider for guidance about when you might try to conceive.
Miscarriage is usually a one-time occurrence. Most women who miscarry go on to have a healthy pregnancy after miscarriage. Less than 5 percent of women have two consecutive miscarriages, and only 1 percent have three or more consecutive miscarriages.
If you experience multiple miscarriages, generally two or three in a row, consider testing to identify any underlying causes. Such causes could include problems with the uterus, blood clotting or chromosomes. If the cause of your miscarriages can't be identified, don't lose hope. About 60 to 80 percent of women with unexplained repeated miscarriages go on to have healthy pregnancies.
Disease Diagnoses
Disease Allopathic Generics
-
Drotaverine
For pain relief. Consume 1/2 pill 3 times a day.
-
Hyoscine Butylbromide
For pain relief. Consume 1/2 pill 3 times a day.
-
Ergometrine Maleate
In case of occasional bleeding, complete rest is required. However, medications containing methyl ergometrine maleate are used to stop the discharge.
Take 2 tablets 2/3 times a day.
-
Ferrous Sulfate
For anemia. Consume 1 capsule 2 times a day after meals.
-
Cephalexin
1 capsule every 6 hours for 5/7 days.
-
Vitamin E [Alpha Tocopherol Acetate]
Medicines containing tocopherol acetate for uterine weakness.
1 pill 2 times a day.
-
Clobazam
Medicines containing clobazam for mental agitation, restlessness, or insomnia.
1 pill in the morning and 1 pill at night.
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Miscarriage (Abortion) and Learn More about Diseases

Albinism

Scarlet fever
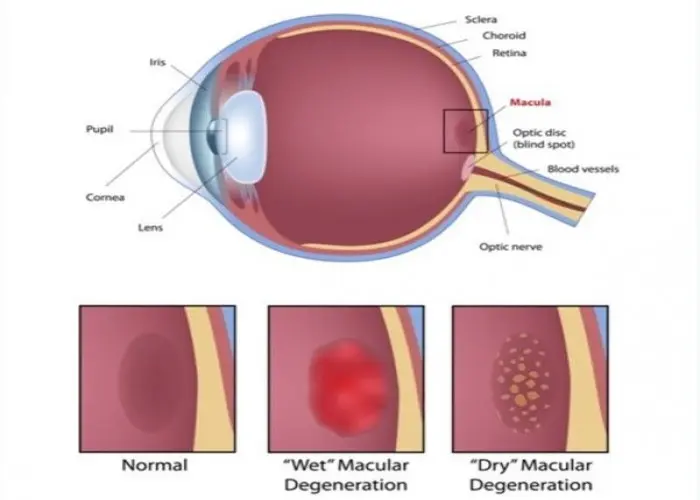
Dry macular degeneration
C. difficile infection
Pediatric brain tumors

Dystonia
Kleptomania

Separation anxiety disorder
Miscarriage, abortion, গর্ভপাত
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
