 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Inflammatory breast cancer

Inflammatory breast cancer (IBC) is a rare and aggressive form of breast cancer that accounts for less than 5% of all breast cancer cases. IBC is called "inflammatory" because the affected breast often appears swollen, red, and warm, resembling an inflammatory reaction, but without any known infection or injury.
IBC differs from other types of breast cancer in its clinical and pathological characteristics, as it tends to grow rapidly and spread to nearby lymph nodes and tissues, even before a noticeable lump can be felt or seen on imaging tests. IBC also has distinct histological features, such as tumor emboli in the lymphatic vessels and dermal lymphatic invasion.
IBC is often diagnosed at a more advanced stage than other types of breast cancer, which makes it harder to treat and has a lower survival rate. However, advances in imaging, biopsy techniques, and systemic therapies, including chemotherapy, targeted therapy, and radiation therapy, have improved the outcomes for some women with IBC. Treatment typically involves a combination of these therapies, followed by surgery and adjuvant therapy to reduce the risk of recurrence.
Due to its rarity and unique features, IBC requires a multidisciplinary team approach and specialized expertise to ensure accurate diagnosis and optimal management. It is important for women to be aware of the signs and symptoms of IBC, such as sudden onset of breast swelling, redness, tenderness, and skin changes, and to seek medical attention promptly if any of these symptoms occur.
Research Papers
Disease Signs and Symptoms
- Breast pain
- Breast lump
- Breast cancer
- Breast tumors
- Swollen breast
- Breast tenderness
- Abnormal breast growth
- Enlarged lymph nodes under the arm, above the collarbone or below the collarbone
Disease Causes
Inflammatory breast cancer
It's not clear what causes inflammatory breast cancer.
Doctors know that inflammatory breast cancer begins when a breast cell develops changes in its DNA. Most often the cell is located in one of the tubes (ducts) that carry breast milk to the nipple. But the cancer can also begin with a cell in the glandular tissue (lobules) where breast milk is produced.
A cell's DNA contains the instructions that tell a cell what to do. The changes to the DNA tell the breast cell to grow and divide rapidly. The accumulating abnormal cells infiltrate and clog the lymphatic vessels in the skin of the breast. The blockage in the lymphatic vessels causes red, swollen and dimpled skin — a classic sign of inflammatory breast cancer.
Disease Prevents
Disease Treatments
Inflammatory breast cancer treatment begins with chemotherapy. If the cancer hasn't spread to other areas of the body, treatment continues with surgery and radiation therapy. If the cancer has spread to other areas of the body, your doctor may recommend other drug treatments in addition to chemotherapy to slow the growth of the cancer.
Chemotherapy
Chemotherapy uses drugs to destroy fast-growing cells, such as cancer cells. You may receive chemotherapy drugs through a vein (intravenously), in pill form or both.
Chemotherapy is used prior to surgery for inflammatory breast cancer. This pre-surgical treatment, referred to as neoadjuvant therapy, aims to shrink the cancer before the operation and increase the chance that surgery will be successful.
If your cancer has a high risk of returning or spreading to another part of your body, your doctor may recommend additional chemotherapy after you've completed other treatments in order to decrease the chance that the cancer will recur.
Surgery
After chemotherapy, you may have an operation to remove the affected breast and some of the nearby lymph nodes. The operation usually includes:
- Surgery to remove the breast (mastectomy). A total mastectomy includes removing all of the breast tissue — the lobules, ducts, fatty tissue and some skin, including the nipple and areola.
- Surgery to remove the nearby lymph nodes. The surgeon will remove the lymph nodes under the arm and near the affected breast (axillary dissection).
Talk with your doctor about your options for breast reconstruction. Surgery to reconstruct the breast is often delayed until after you complete all of your breast cancer treatments.
Radiation therapy
Radiation therapy uses high-powered beams of energy, such as X-rays or protons, to kill cancer cells. Radiation therapy is typically done using a large machine that aims the energy beams at your body (external beam radiation).
For inflammatory breast cancer, radiation therapy is used after surgery to kill any cancer cells that might remain. The radiation is aimed at your chest, armpit and shoulder.
Targeted therapy
Targeted drug treatments attack specific abnormalities within cancer cells. As an example, several targeted therapy drugs focus on a protein that some breast cancer cells overproduce called human epidermal growth factor receptor 2 (HER2). The protein helps breast cancer cells grow and survive. By targeting cells that make too much HER2, the drugs can damage cancer cells while sparing healthy cells.
If your inflammatory breast cancer cells test positive for HER2, your doctor might recommend combining targeted therapy with your initial chemotherapy treatment. After surgery, targeted therapy can be combined with hormone therapy.
For cancer that spreads to other parts of the body, targeted therapy drugs that focus on other abnormalities within cancer cells are available. Your cancer cells may be tested to see which targeted therapies might be helpful for you.
Hormone therapy
Hormone therapy — perhaps more properly termed hormone-blocking therapy — is used to treat breast cancers that use your hormones to grow. Doctors refer to these cancers as estrogen receptor positive (ER positive) and progesterone receptor positive (PR positive) cancers.
Hormone therapy can be used after surgery or other treatments to decrease the chance of your cancer returning. If the cancer has already spread, hormone therapy may shrink and control it.
Treatments that can be used in hormone therapy include:
- Medications that block hormones from attaching to cancer cells (selective estrogen receptor modulators)
- Medications that stop the body from making estrogen after menopause (aromatase inhibitors)
- Surgery or medications to stop hormone production in the ovaries
Immunotherapy
Immunotherapy uses your immune system to fight cancer. Your body's disease-fighting immune system may not attack your cancer because the cancer cells produce proteins that help them hide from the immune system cells. Immunotherapy works by interfering with that process.
Immunotherapy might be an option if your cancer has spread to other areas of the body and is triple negative, which means that the cancer cells don't have receptors for estrogen, progesterone or HER2. Your doctor may test your cancer cells to see if they're likely to respond to immunotherapy.
Supportive (palliative) care
Palliative care is specialized medical care that focuses on providing relief from pain and other symptoms of a serious illness. Palliative care specialists work with you, your family and your other doctors to provide an extra layer of support that complements your ongoing care. Palliative care can be used while undergoing other aggressive treatments, such as surgery, chemotherapy or radiation therapy.
When palliative care is used along with all of the other appropriate treatments, people with cancer may feel better and live longer.
Palliative care is provided by a team of doctors, nurses and other specially trained professionals. Palliative care teams aim to improve the quality of life for people with cancer and their families. This form of care is offered alongside curative or other treatments you may be receiving.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Inflammatory breast cancer and Learn More about Diseases
Primary sclerosing cholangitis
Testicular cancer
Polyhydramnios

Premature ejaculation

Carbon monoxide poisoning
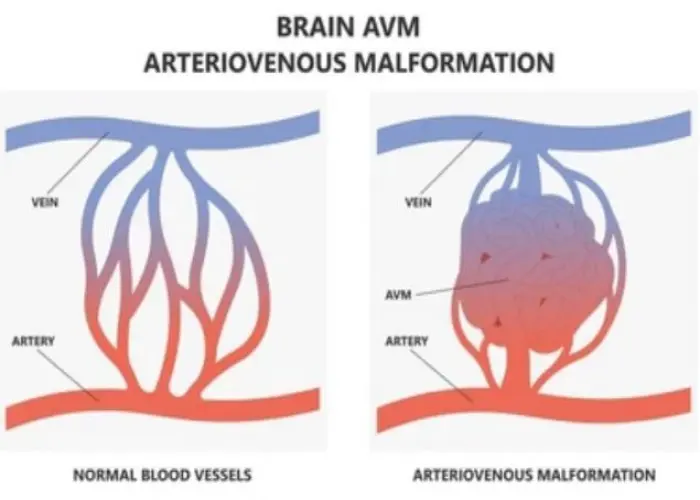
Arteriovenous malformation

Food poisoning
Brain aneurysm
inflammatory breast cancer, ibc, প্রদাহজনক স্তন ক্যান্সার, আইবিসি
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
