 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Inflammatory bowel disease (IBD)

Inflammatory bowel disease (IBD) is a chronic disorder characterized by inflammation of the digestive tract. The two main types of IBD are Crohn's disease and ulcerative colitis, both of which can cause severe abdominal pain, diarrhea, fatigue, weight loss, and other symptoms.
Crohn's disease can affect any part of the digestive tract, from the mouth to the anus, and can cause inflammation in multiple areas. Ulcerative colitis, on the other hand, primarily affects the large intestine (colon) and the rectum.
The exact cause of IBD is unknown, but it is thought to be an autoimmune disorder in which the body's immune system mistakenly attacks the lining of the digestive tract. Other factors that may contribute to the development of IBD include genetic predisposition, environmental factors, and an imbalance in the gut microbiome.
Treatment for IBD typically involves a combination of medication and lifestyle changes, such as:
- Anti-inflammatory drugs to reduce inflammation and manage symptoms
- Immune system suppressors to reduce the body's immune response
- Antibiotics to treat infections or other complications
- Probiotics to restore a healthy balance of bacteria in the gut
- Dietary changes to avoid trigger foods and maintain adequate nutrition
- Surgery in severe cases or if medication and lifestyle changes are not effective
While there is no cure for IBD, many people with the condition are able to manage their symptoms and achieve remission with appropriate treatment. It is important to work closely with a healthcare provider to develop a personalized treatment plan and monitor the condition for any potential complications.
Research Papers
Disease Signs and Symptoms
- Diarrhea
- Fatigue (Tiredness)
- Abdomen pain
- Abdomen cramps
- Blood in stool
- Loss of appetite
- Weight loss
Disease Causes
Inflammatory bowel disease (IBD)
The exact cause of inflammatory bowel disease remains unknown. Previously, diet and stress were suspected, but now doctors know that these factors may aggravate but aren't the cause of IBD.
One possible cause is an immune system malfunction. When your immune system tries to fight off an invading virus or bacterium, an abnormal immune response causes the immune system to attack the cells in the digestive tract, too. Heredity also seems to play a role in that IBD is more common in people who have family members with the disease. However, most people with IBD don't have this family history.
Disease Prevents
Disease Treatments
The goal of inflammatory bowel disease treatment is to reduce the inflammation that triggers your signs and symptoms. In the best cases, this may lead not only to symptom relief but also to long-term remission and reduced risks of complications. IBD treatment usually involves either drug therapy or surgery.
Anti-inflammatory drugs
Anti-inflammatory drugs are often the first step in the treatment of inflammatory bowel disease. Anti-inflammatories include corticosteroids and aminosalicylates, such as mesalamine (Asacol HD, Delzicol, others), balsalazide (Colazal) and olsalazine (Dipentum). Which medication you take depends on the area of your colon that's affected.
Immune system suppressors
These drugs work in a variety of ways to suppress the immune response that releases inflammation-inducing chemicals into the body. When released, these chemicals can damage the lining of the digestive tract.
Some examples of immunosuppressant drugs include azathioprine (Azasan, Imuran), mercaptopurine (Purinethol, Purixan) and methotrexate (Trexall).
Biologics
Biologics are a newer category of therapy in which therapy is directed toward neutralizing proteins in the body that are causing inflammation. Some are administered via intravenous (IV) infusions and others are injections you give yourself. Examples include infliximab (Remicade), adalimumab (Humira), golimumab (Simponi), certolizumab (Cimzia), vedolizumab (Entyvio) and ustekinumab (Stelara).
Antibiotics
Antibiotics may be used in addition to other medications or when infection is a concern — in cases of perianal Crohn's disease, for example. Frequently prescribed antibiotics include ciprofloxacin (Cipro) and metronidazole (Flagyl).
Other medications and supplements
In addition to controlling inflammation, some medications may help relieve your signs and symptoms, but always talk to your doctor before taking any over-the-counter medications. Depending on the severity of your IBD, your doctor may recommend one or more of the following:
- Anti-diarrheal medications. A fiber supplement — such as psyllium powder (Metamucil) or methylcellulose (Citrucel) — can help relieve mild to moderate diarrhea by adding bulk to your stool. For more-severe diarrhea, loperamide (Imodium A-D) may be effective.
- Pain relievers. For mild pain, your doctor may recommend acetaminophen (Tylenol, others). However, ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve) and diclofenac sodium likely will make your symptoms worse and can make your disease worse as well.
- Vitamins and supplements. If you're not absorbing enough nutrients, your doctor may recommend vitamins and nutritional supplements.
Nutritional support
When weight loss is severe, your doctor may recommend a special diet given via a feeding tube (enteral nutrition) or nutrients injected into a vein (parenteral nutrition) to treat your IBD. This can improve your overall nutrition and allow the bowel to rest. Bowel rest can reduce inflammation in the short term.
If you have a stenosis or stricture in the bowel, your doctor may recommend a low-residue diet. This will help to minimize the chance that undigested food will get stuck in the narrowed part of the bowel and lead to a blockage.
Surgery
If diet and lifestyle changes, drug therapy, or other treatments don't relieve your IBD signs and symptoms, your doctor may recommend surgery.
- Surgery for ulcerative colitis. Surgery involves removal of the entire colon and rectum and the production of an internal pouch attached to the anus that allows bowel movements without a bag.
- In some cases a pouch is not possible. Instead, surgeons create a permanent opening in your abdomen (ileal stoma) through which stool is passed for collection in an attached bag.
- Surgery for Crohn's disease. Up to two-thirds of people with Crohn's disease will require at least one surgery in their lifetime. However, surgery does not cure Crohn's disease.
- During surgery, your surgeon removes a damaged portion of your digestive tract and then reconnects the healthy sections. Surgery may also be used to close fistulas and drain abscesses.
- The benefits of surgery for Crohn's disease are usually temporary. The disease often recurs, frequently near the reconnected tissue. The best approach is to follow surgery with medication to minimize the risk of recurrence.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Inflammatory bowel disease (IBD) and Learn More about Diseases

Tennis elbow

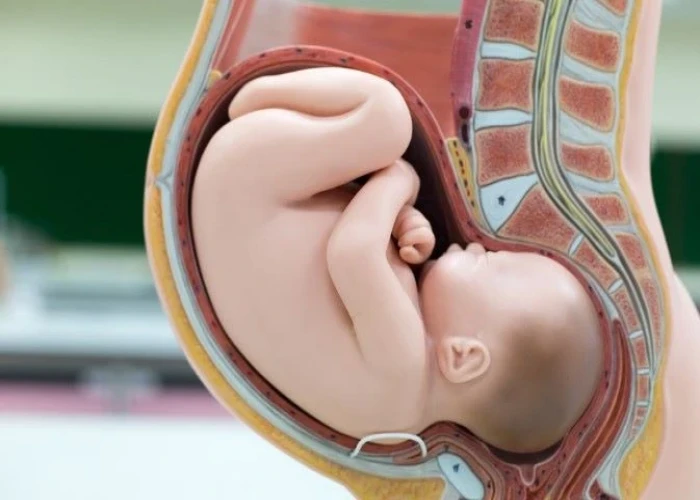
Preterm labor

N/A
Polyhydramnios

Chronic cough

Sprains
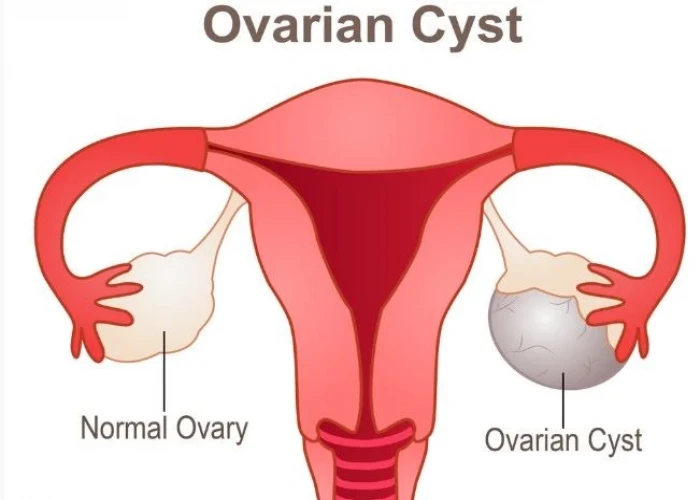
Ovarian cysts

MRSA infection
inflammatory bowel disease, ibd, প্রদাহজনক পেটের রোগ, আইবিডি
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
