Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
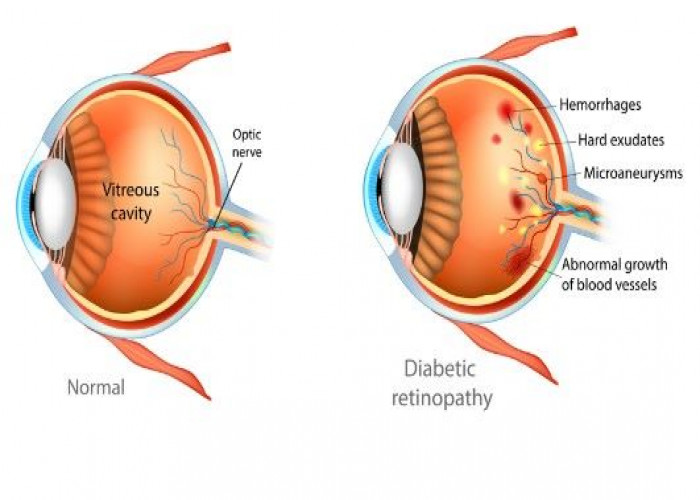
Diabetic retinopathy
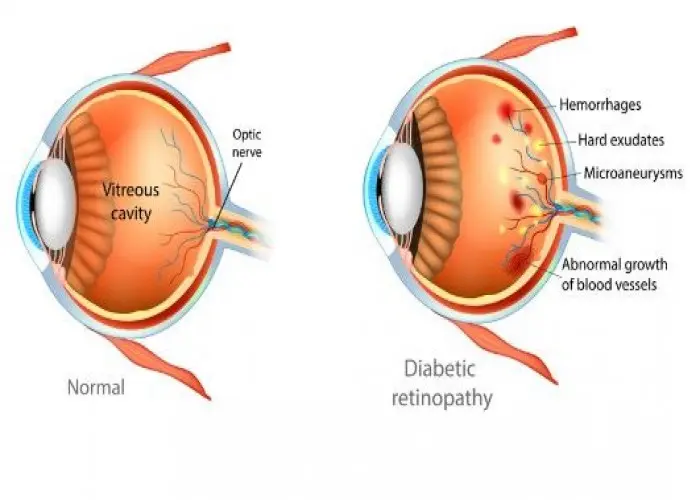
Diabetic retinopathy is a complication of diabetes that affects the eyes. It is caused by damage to the blood vessels in the retina, the light-sensitive tissue at the back of the eye. High blood sugar levels over time can cause the blood vessels to weaken and leak, leading to swelling and growth of abnormal blood vessels. These changes can cause vision problems and even blindness if left untreated.
Diabetic retinopathy typically develops gradually and may not cause noticeable symptoms in the early stages. However, as the condition progresses, symptoms such as blurred or distorted vision, dark spots or floaters in the vision, or difficulty seeing at night may occur.
There are two types of diabetic retinopathy: nonproliferative and proliferative. Nonproliferative diabetic retinopathy is the early stage of the disease, and is characterized by weakened and leaky blood vessels in the retina. Proliferative diabetic retinopathy is a more advanced stage, where new, abnormal blood vessels grow in the retina. These new blood vessels can leak and cause scarring, leading to more severe vision problems.
Preventing diabetic retinopathy involves proper diabetes management, including regular monitoring of blood sugar levels and maintaining a healthy lifestyle. People with diabetes should also have regular eye exams to check for any signs of retinopathy. Treatment of diabetic retinopathy may include laser surgery to seal leaking blood vessels or to prevent the growth of abnormal blood vessels. In advanced cases, surgery may be necessary to remove scar tissue or to restore vision.
In conclusion, diabetic retinopathy is a serious complication of diabetes that can lead to vision problems and blindness if left untreated. By managing your diabetes and taking steps to prevent complications, you can help protect your eye health and prevent vision loss. If you have diabetes, it is important to have regular eye exams to check for any signs of retinopathy. If you experience any symptoms of diabetic retinopathy, seek medical attention immediately.
Research Papers
Disease Signs and Symptoms
- Blurred vision of eye
- Fluctuating vision
- High blood sugar
- Diabetes
- Dark or empty areas in vision
Disease Causes
Diabetic retinopathy
Over time, too much sugar in your blood can lead to the blockage of the tiny blood vessels that nourish the retina, cutting off its blood supply. As a result, the eye attempts to grow new blood vessels. But these new blood vessels don't develop properly and can leak easily.
There are two types of diabetic retinopathy:
- Early diabetic retinopathy. In this more common form — called nonproliferative diabetic retinopathy (NPDR) — new blood vessels aren't growing (proliferating).
- When you have NPDR, the walls of the blood vessels in your retina weaken. Tiny bulges protrude from the walls of the smaller vessels, sometimes leaking fluid and blood into the retina. Larger retinal vessels can begin to dilate and become irregular in diameter as well. NPDR can progress from mild to severe as more blood vessels become blocked.
- Sometimes retinal blood vessel damage leads to a buildup of fluid (edema) in the center portion (macula) of the retina. If macular edema decreases vision, treatment is required to prevent permanent vision loss.
- Advanced diabetic retinopathy. Diabetic retinopathy can progress to this more severe type, known as proliferative diabetic retinopathy. In this type, damaged blood vessels close off, causing the growth of new, abnormal blood vessels in the retina. These new blood vessels are fragile and can leak into the clear, jellylike substance that fills the center of your eye (vitreous).
- Eventually, scar tissue from the growth of new blood vessels can cause the retina to detach from the back of your eye. If the new blood vessels interfere with the normal flow of fluid out of the eye, pressure can build in the eyeball. This buildup can damage the nerve that carries images from your eye to your brain (optic nerve), resulting in glaucoma.
Disease Prevents
Diabetic retinopathy
You can't always prevent diabetic retinopathy. However, regular eye exams, good control of your blood sugar and blood pressure, and early intervention for vision problems can help prevent severe vision loss.
If you have diabetes, reduce your risk of getting diabetic retinopathy by doing the following:
- Manage your diabetes. Make healthy eating and physical activity part of your daily routine. Try to get at least 150 minutes of moderate aerobic activity, such as walking, each week. Take oral diabetes medications or insulin as directed.
- Monitor your blood sugar level. You might need to check and record your blood sugar level several times a day — or more frequently if you're ill or under stress. Ask your doctor how often you need to test your blood sugar.
- Ask your doctor about a glycosylated hemoglobin test. The glycosylated hemoglobin test, or hemoglobin A1C test, reflects your average blood sugar level for the two- to three-month period before the test. For most people with diabetes, the A1C goal is to be under 7%.
- Keep your blood pressure and cholesterol under control. Eating healthy foods, exercising regularly and losing excess weight can help. Sometimes medication is needed, too.
- If you smoke or use other types of tobacco, ask your doctor to help you quit. Smoking increases your risk of various diabetes complications, including diabetic retinopathy.
- Pay attention to vision changes. Contact your eye doctor right away if your vision suddenly changes or becomes blurry, spotty or hazy.
Remember, diabetes doesn't necessarily lead to vision loss. Taking an active role in diabetes management can go a long way toward preventing complications.
Disease Treatments
Treatment, which depends largely on the type of diabetic retinopathy you have and how severe it is, is geared to slowing or stopping the progression.
Early diabetic retinopathy
If you have mild or moderate nonproliferative diabetic retinopathy, you might not need treatment right away. However, your eye doctor will closely monitor your eyes to determine when you might need treatment.
Work with your diabetes doctor (endocrinologist) to determine if there are ways to improve your diabetes management. When diabetic retinopathy is mild or moderate, good blood sugar control can usually slow the progression.
Advanced diabetic retinopathy
If you have proliferative diabetic retinopathy or macular edema, you'll need prompt treatment. Depending on the specific problems with your retina, options might include:
- Injecting medications into the eye. These medications, called vascular endothelial growth factor inhibitors, are injected into the vitreous of the eye. They help stop growth of new blood vessels and decrease fluid buildup.
- Two drugs are approved by the U.S. Food & Drug Administration (FDA) for treatment of diabetic macular edema — ranibizumab (Lucentis) and aflibercept (Eylea). A third drug, bevacizumab (Avastin), can be used off-label for the treatment of diabetic macular edema.
- These drugs are injected using topical anesthesia. The injections can cause mild discomfort, such as burning, tearing or pain, for 24 hours after the injection. Possible side effects include a buildup of pressure in the eye and infection.
- These injections will need to be repeated. In some cases, the medication is used with photocoagulation.
- Photocoagulation. This laser treatment, also known as focal laser treatment, can stop or slow the leakage of blood and fluid in the eye. During the procedure, leaks from abnormal blood vessels are treated with laser burns.
- Focal laser treatment is usually done in your doctor's office or eye clinic in a single session. If you had blurred vision from macular edema before surgery, the treatment might not return your vision to normal, but it's likely to reduce the chance of the macular edema worsening.
- Panretinal photocoagulation. This laser treatment, also known as scatter laser treatment, can shrink the abnormal blood vessels. During the procedure, the areas of the retina away from the macula are treated with scattered laser burns. The burns cause the abnormal new blood vessels to shrink and scar.
- It's usually done in your doctor's office or eye clinic in two or more sessions. Your vision will be blurry for about a day after the procedure. Some loss of peripheral vision or night vision after the procedure is possible.
- Vitrectomy. This procedure uses a tiny incision in your eye to remove blood from the middle of the eye (vitreous) as well as scar tissue that's tugging on the retina. It's done in a surgery center or hospital using local or general anesthesia.
While treatment can slow or stop the progression of diabetic retinopathy, it's not a cure. Because diabetes is a lifelong condition, future retinal damage and vision loss are still possible.
Even after treatment for diabetic retinopathy, you'll need regular eye exams. At some point, you might need additional treatment.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Diabetic retinopathy and Learn More about Diseases
Heart disease

Rheumatic fever
Sweating and body odor

Neurofibromatosis
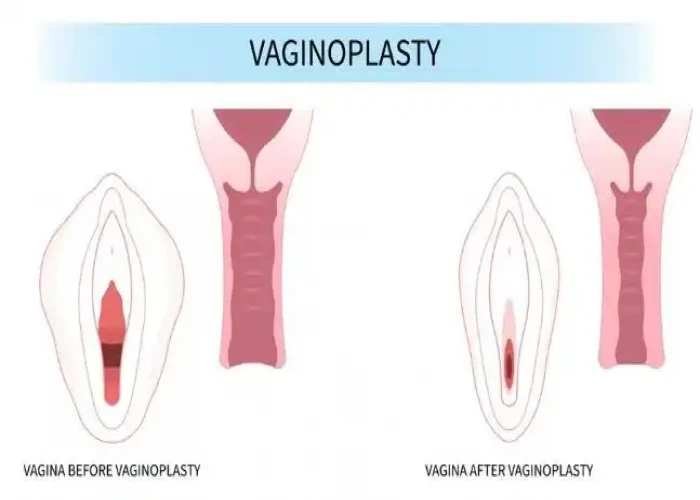
Vaginal agenesis

Arteriovenous fistula
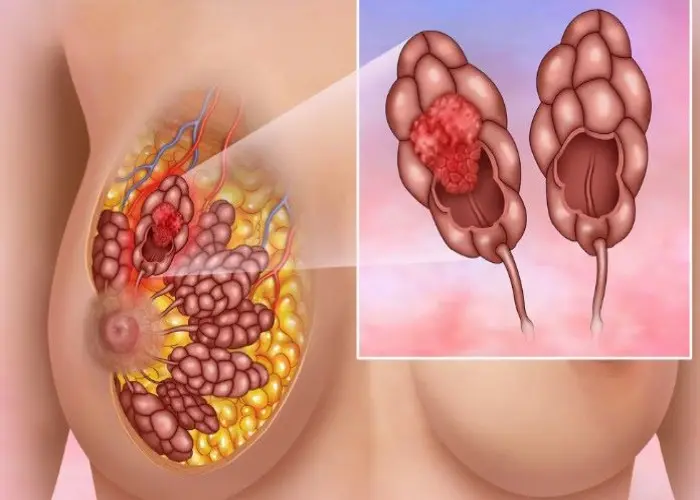
Invasive lobular carcinoma

Pancreatitis
diabetic retinopathy, ডায়াবেটিক রেটিনা ক্ষয়
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.